Research Article
Treatment of Early Gestational Glucose Intolerance
V Seshiah 1, Pikee Saxena 2, Anjalakshi C 3, N. Bhavatharani 4, Geetha Lakshmi 5, B Madhuri 6, Rajesh Jain 7*
1Hony Distinguished professor, Department of Medicine Tamilnadu Dr. MGR. Medical University Chennai, India; 2Obstetrics and Gynaecology, LHMC New Delhi, India; 3Obstetrics and Gynaecology, Madha Medical College and Research Institute Chennai, IND; 4Research Society for Study of Diabetes in India, Erode, India; 5Obstetrics and Gynaecology, Madras Medical College, Chennai, IND; 6Member, Research Society for Study of Diabetes in India, Erode, India; 7*Department of Medicine, Jain Hospital & Research Centre, Kanpur, India
Corresponding Author: Rajesh Jain MD, Consultant, Jain Hospital & Research Centre, Kanpur, India; Email: [email protected]
Abstract
Aim: This study aims to determine the risk of gestational diabetes mellitus (GDM) in the first trimester at 8 weeks based on the 2-hour postprandial blood glucose (2-hour PPBG) levels and assess the risk of GDM with intervention Interventionmin.
Methodology: This study was conducted in two centers, with 182 pregnant women in Group A, 100 in Group B, and 69 in Group C. The participants were screened at 8-10 weeks, and DIPSI tests were performed to check for GDM development.
Results: In Group A, when the 2-hour PPBG was less than 110 mg/dl, only 4% and 1.2% of participants developed GDM in Study 1 and Study 2, respectively. For Group B, 95.9% of the participants developed GDM with a 2-hour postprandial blood sugar of ≥110 mg/dl and no intervention. However, in Group C with Metformin intervention, only 1.4% of the women developed GDM.
Key Words: EGGI; GDM; PPBG; DIPSI
Diabetes mellitus is a rapidly evolving pandemic and a significant public health problem in recent decades [1]. It affects millions of people worldwide, significantly impacting the quality of their lives. Efforts are underway globally to detect diabetes in its early stages and prevent its complications [2].
Detection of diabetes does not mean prevention of diabetes.
We need primary diabetes prevention [3]—the disease should not develop. To achieve a diabetes-free generation, Lise Kingo suggested focusing on “Female Gende” as the Key to Diabetes Prevention,” based on de”elopmental origin. At fertilization, only the spermatozoa’sspermatozoa’srs the ovum, and all the cytoplasm, mitochondria, and mitochondrial DNA are maternally inherited. Embryology of Beta Cell Development Each islet cell in the developing fetus functions as an endocrine organ. Pancreatic islets differentiate at the 10th & 11th weeks of gestation and recognize and respond to maternal glycemia at 11 weeks [4]. If the prandial glycaemic level is abnormal at this crucial time, it will stimulate increased beta cell secretion of insulin.
Intrauterine Programming Gestational programming is a process whereby stimuli, maternal fuels, or stresses that occur at critical or sensitive periods of fetal development permanently change the structure, physiology, and metabolism, predisposing individuals to disease in adult life. A good example is gestational diabetes mellitus (GDM). “Fetal Origin” of Adult Disease,” as opined by” David Barker [5,6], suggests that major developmental events in the natural history of non-communicable diseases (NCDs) begin in utero. Hence, there is a need to “Focus on the”Fetus for the Future” to achieve ” diabetes-free generation, as suggested by author Seshiah. Also, his opinion is that “GDM is the m”ther of Non-Communicable Diseases.” In addition,” exposure to a hyperglycaemic environment in utero is associated with an increased occurrence of impaired glucose intolerance and dysfunctional insulin response in young offspring, independent of genetic predisposition to type 2 DM [7]. Even though one might have a genetic predisposition for diabetes, that person should be exposed to epigenetic factors, such as intrauterine or extrauterine [8]. The intrauterine factor (environment) is dominant [9]. This manifestation is simply explained as “Genetics loa”s the gun, and environment triggers it off,” without”genetic factors, the intrauterine environment can cause disease.
Detection and Prediction of GDM Detection of GDM is possible with 2hr PG ≥ 140 mg/dl. The most important concern is predicting GDM to prevent its development and consequences [10]. A National Institute of Health (NIH) study in 2018 suggested that HBA1c 5.3 (2hr Postprandial Blood Glucose (PPBG) >110 mg/dl) in the 10th week predicts GDM [11]. Still, no explanation has been given for predicting or preventing GDM.
Conceptualization
Maternal 2hr PPBG should not cross >110 mg/dl at the 10th week as fetal beta cells start secreting insulin around the 11th week of Pregnancy. 2hPregnancyandial Blood Glucose (PPBG) at the 10th week > 110 mg/dl predicts GDM; hence, blood glucose must be brought to <110 mg/dl before 11 weeks as Fetal Beta starts secreting insulin around 10-11 weeks, with Fetal insulin secretion, changes in maternal metabolism start.
Guidelines to Screen glucose intolerance at appropriate Gestational weeks:
Prediction of GDM can be done if 2hr PPBG≥110 mg/dl at 10th week. At the 8th week itself, PPBG needs to be estimated because, in case PPBG is > 110 mg/dl at this week, a grace period of 2 weeks is available to bring it down to PPBG <110 mg/dl at the 10th week with metformin 250 mg twice a day, in addition to MNT and exercise. Instead, when PPBG is estimated at the 10th week and if it is>110 mg/dl, insufficient time will be available to achieve PPBG<110 mg/dl in the 11th week, so fetal beta cell insulin secretion starts to increase. If PPBG is < 110 mg/dl at the 10th week, no increase in fetal beta cell insulin secretion occurs at the 11th week of gestation.
Metformin is safe for use throughout Pregnancy.
MePregnancyas is approved as the first oral anti-diabetic medication to be used safely from conception to confinement to lower the risk of pregnancy-induced hypertension and pre-eclampsia [12]. The Lancet Diabetes & Endocrinology also showed no difference in weight, height, head, and waist circumference in children born to mothers treated with Metformin and placebo. Metformin exposure in utero is not linked to higher BMI for children of women with diabetes [13] and is safe. The ethics committee of Lady Hardinge Medical College and Madras Medical College has approved the administration of Metformin for the study.
Objective. To determine the risk of GDM in the I trimester at 8 weeks when 2hr PPBG is <110 mg% (Group A). To assess the risk of GDM in the I Trimester at 8 weeks when 2hr PPBG is >110 mg% (Group B) without intervention
Intervention in the risk of GDM in the I Trimester at 8 weeks when 2hr PPBG is>110mg% with intervention Interventionroup (C)
Methodology: A Prospective study in two centers; Group A, 182 pregnant women; Group B, 100; and Group C, 69. They were screened for 8-10 weeks, and DIPSI tests were done to determine how many developed GDM.
Table 1 Post Prandial Blood Sugar in Study 1 and Study 2 and Group A, Group B, and Group C conversion to GDM
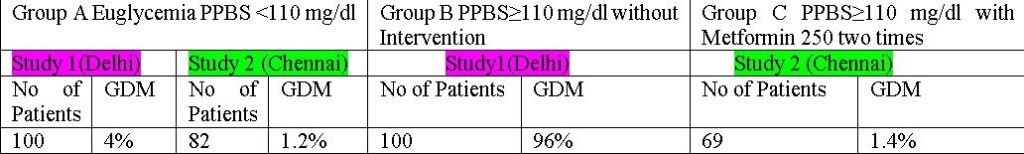
Results: In Study 1 and Study 2 of Group A, less than 110 mg/dl, only 4% and 1.2% developed GDM, respectively. In Group B and Group C, if 2-hour postprandial blood sugar is ≥110 mg/dl and no intervention in Group B study, 95.9% developed GDM. In the intervention Group C, only 1.4% of women developed GDM, and that too because one woman discontinued Metformin after 6 months of gestation, which clearly shows there is great potential for preventing GDM and NCDs.
.
“Conclusion – “Scope for Prevention of Diabetes: Gestational diabetes mellitus (GDM) can be predicted when the 2-hour postprandial blood glucose (PPBG) level is greater than 110 mg/dl at the 10th week of pregnancy. To PregnancyDM, action should be taken by the 8th week to maintain the maternal 2-hour PPBG levels between 99-109 mg/dl throughout the pregnancy. To Pregnancyr a “Diabetes Free” Generation,” the focus “should be directed towards the development of the offspring, with a specific emphasis on fetal health for future generations [14]. Early Gestational Glucose Intolerance (EGGI) is characterized by elevated 2-hour PPBG levels in the early weeks of pregnancy (10 Pregnancy is recognized as EGGI. The concept of primordial prevention of diabetes has been validated through preliminary studies at LHMC, Delhi, and MMC, Chennai. The positive outcomes of these studies demonstrate the possibility of primordial diabetes prevention.”
References
“. International Diabetes Federation. IDF Diabetes Atlas, 10th ed. Brussels, Belgium: 2021. Available at: https://www.diabetesatlas.org.
2. Briana Mezuk, Julie Ober Allen; Rethinking the Goals of Diabetes Prevention Programs. Diabetes Care. 1 November 2021; 44 (11): 2457–2459. https://doi.org/10.2337/dci21-0038.
3. Seshiah, V. Primordial prevention: a futuristic approach to intervene in gestational diabetes and its sequelae. Int J Diabetes Dev Ctries 43, 483–484 (2023). https://doi.org/10.1007/s13410-023-01216-1.
4. Piper K, Brickwood S, Turnpenny LW, et al.: Beta cell differentiation during early human pancreas development. J Endocrinol. 2004; 181:11-23. 10.1677/joe.0.1810011.
5. K, Devaskar SU: Fetal origins of adult disease. Curr Probl Pediatr Adolesc Health Care. 2011; 41:158-76. 10.1016/j.cppeds.2011.01.001.
6. Lucas A, Fewtrell MS, Cole TJ: Fetal origins of adult disease hypothesis revisited. BMJ. 1999; 24:245-9. 10.1136/bmj.319.7204.245.
7. Sobngwi E, Boudou P, Mauvais-Jarvis F, et al.: Effect of a diabetic environment in utero on predisposition to type 2 diabetes. Lancet. 2003; 361:1861-1865. 10.1016/S0140-6736(03)13505-2.
8. Gill-Randall R, Adams D, Ollerton RL, et al.: Type 2 diabetes mellitus — genes or intrauterine environment? An embryo transfer paradigm in rats. Diabetologia. 2004; 47:1354-1359. 10.1007/s00125-004- 1464-x.
9. Goyal D, Limesand SW, Goyal R. Epigenetic responses and the developmental origins of health and disease. J Endocrinol. 2019 Jul 1;242(1): T105-T119. doi: 10.1530/JOE-19-0009
10. Seshiah V, Bronson SC, Balaji V, Jain R, Anjalakshi C: Prediction and Prevention of Gestational Diabetes Mellitus and Its Sequelae by Administering Metformin in the Early Weeks of Pregnancy. Cureus. 2022; 15:31532. 10.7759/cureus.31532.
11. Hinkle SN, Tsai MY, Rawal S, Albert PS, Zhang C. HbA1c Measured in the First Trimester of Pregnancy and the Association with Gestational Diabetes. Sci Rep. 2018 Aug 16;8(1):12249. doi: 10.1038/s41598-018-30833-8.
12. Brand KMG, Saarelainen L, Sonajalg J, Boutmy E, Foch C, Vääräsmäki M, Morin-Papunen L, Schlachter J; CLUE Study Group; Hakkarainen KM, Korhonen P. Metformin in pregnancy and risk of adverse long-term outcomes: a register-based cohort study. BMJ Open Diabetes Res Care. 2022 Jan;10(1): e002363. doi: 10.1136/bmjdrc-2021-002363
13. Linh Nguyen, Shiao-Yng Chan, Adrian Kee Keong Teo: Metformin from mother to unborn child – Are there unwarranted effects? EBioMedicine. 2018; 35:394-404. 10.1016/j.ebiom.2018.08.047.
14. Bronson SC, Seshiah V: Transgenerational Transmission of Non-communicable Diseases: How to Break the Vicious Cycle? Cureus. 2021; 13:18754. 10.7759/cureus.18754.
- Acknowledgment
Not applicable
- Funding
Not applicable
- Informed Consent
Not applicable
- Conflict of Interest Statement
All the authors declared “No Conflict of Interest” with this publication
- Additional Information: The article is Open Access and is licensed under a Creative Commons Attribution 4.0 International License.
- visit http://creativecommons.org/licenses/by/4.0/
Not applicable
- DOI: 10.62996/daj.30102024
- Cite this Article
V Seshiah 1, Pikee Saxena 2, Anjalakshi C 3, N. Bhavatharani 4, Geetha Lakshmi 5, B Madhuri 6, Rajesh Jain.7* Treatment Early Gestational Glucose Intolerance. Diabetes Asia Journal. 2024; 1(2):19-22. https://doi.org/10.62996/daj.30102024

