Rajesh Jain1 , Veeraswamy Seshiah2
1Dr Rajesh Jain MD chair, Diabetes Asia, Jain hospital & Research Centre, kanpur-208007, India. Email: [email protected]; 2Veeraswamy Seshiah MD, Distinguished Professor of The Tamilnadu MGR Medical University, Chennai, India.
India is one of the countries with diabetes in the world and has one of the highest rates of GDM in women, affecting more than 5 million women in the country each year [1].
India currently has the second highest number of people with type 2 diabetes in the world at 77 million; Almost half of these patients are women. IDF 2019 estimates that 6 million newborns in India alone are affected by some form of hyperglycemia (HIP) during pregnancy, 90% of which are due to GDM [1]. Therefore, all women should be tested for gestational diabetes, even if they are asymptomatic. Unfortunately, the diagnostic criteria are not the same. (Table-1)
Table 1 Diagnostic criteria used by Organizations for estimating hyperglycemia in pregnancy
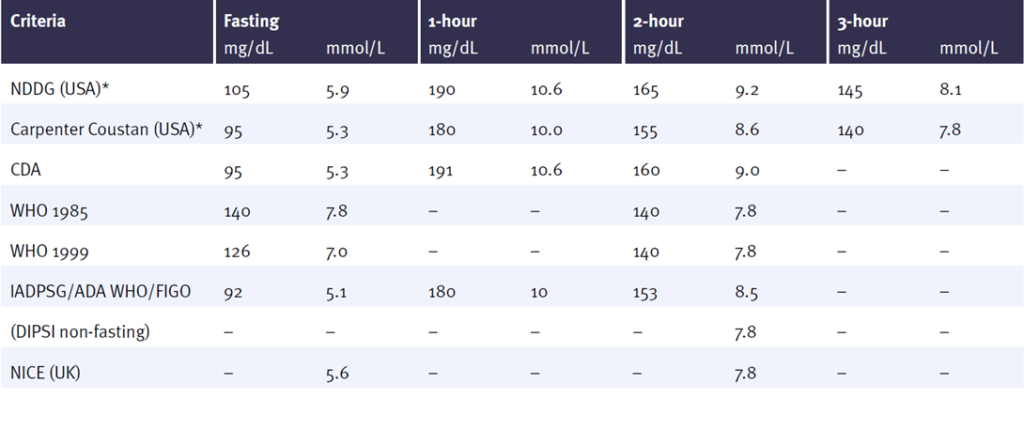
ADA = American Diabetes Association; NDDG = National Diabetes Data Group; CDA = Canadian Diabetes Association; DIPSI = Diabetes in Pregnancy Society of India; WHO = World Health Organization; IADPSG = International Association of the Diabetes and Pregnancy Study Groups. NICE = National Institute for Clinical Excellence; FIGO = International Federation of Gynaecology and Obstetrics* after 50g glucose challenge test-if positive, uses 100g glucose load; at least two need to be positive
(The Sourced from the IDF Atlas 2021)
The global diabetes epidemic is on the rise. According to IDF Head Professor Andrew Boulton, diabetes has become an epidemic.
The global prevalence of diabetes is estimated to rise from 537 million in 2021 to 783 million in 2045, an increase of 46%. [1] Diabetes is common worldwide, and this is a concern; by 2021, there will be 74.1 million diabetics in India (Map 1).
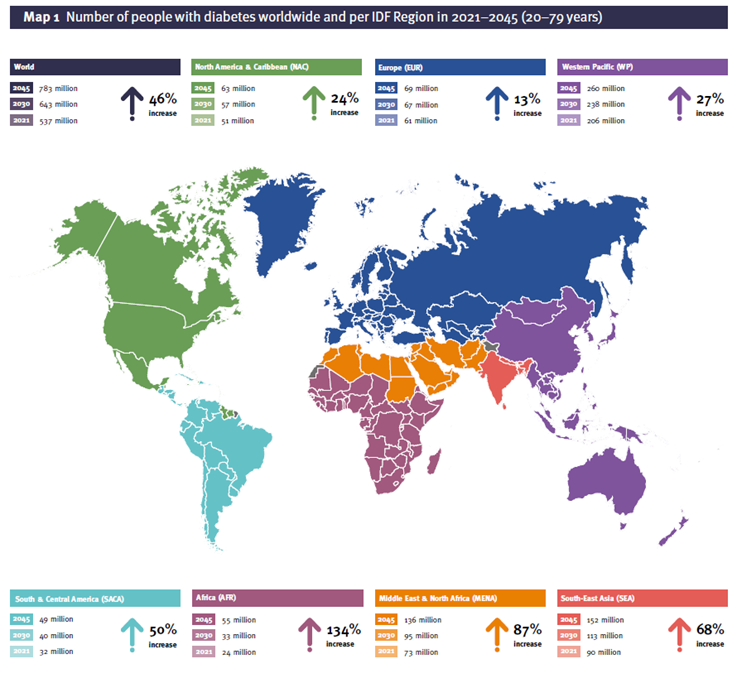
Credit IDF 2021
This increase may be due to the aging of the Population, physical inactivity, urbanization, and obesity. These conditions increase the risk of diabetes mellitus, but early life is a risk factor. As suggested in David Baker’s “Fetal origins of adult disease” hypothesis, pregnancy planning can significantly impact adult health and disease. Pregnancy can be defined as the process in which stress or stimulus during a sensitive or important period of fetal development permanently changes the structure, body, and metabolism and thus creates a predisposition to a disease in the elderly. Lifestyle changes and medical interventions have been reported to slow or delay the development of Type-2 diabetes mellitus in people affected by impaired glucose tolerance (IGT), the first line of defence. Maintaining normoglycemia in GDM or other vulnerable individuals is the best option to prevent developing type 2 diabetes (T2DM). Diabetes can be reversed or stopped through primary prevention. For primary prevention of diabetes mellitus, women with gestational diabetes (GDM) are considered an ideal group because their children are more likely to have diabetes, and most of them acquired T2DM. Gestational diabetes may be an important factor in diabetes and obesity.
By 2021, the Global prevalence of hyperglycaemia in pregnancy (HIP) will be 21.1 million people, accounting for 16.7% of births to women aged 20-49. These individuals may experience some form of hyperglycaemia during pregnancy; 80.3% of these were due to GDM [2].
Therefore, all women must be tested for GDM, even if they have no symptoms.
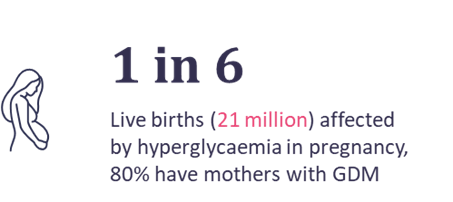
Figure 1 IDF atlas, 2021
The global epidemic of diabetes and hyperglycaemia in pregnancy (HIP) is causing many problems, some of which differ from country to country. A narrow solution is essential to solving these particular problems. In India, the MOHFW Ministry of Health Family Welfare and FOGSI have assisted medical personnel and physicians throughout the HIP management process, working with national groups such as the DIPSI Diabetes in Pregnancy Study Group India, FOGSI Federation of Obstetrics & Gynaecology Society and International organizations such as WDF, IDF, and FIGO who have imparted capacity building of health care professional at Districts and block level with Ministry of health family welfare and states Govt for screening and management of GDM, This multifaceted approach helps solve some multifaceted problems unique to India.
Keywords: Gestational Diabetes Mellitus; Epidemiological Studies; South Asia, Prevalence, Hyperglycaemia in pregnancy, HIP, GDM, FOGSI Federation of Obstetrics and Gynaecology of India.
1. Introduction
Although gestational diabetes mellitus (DIP) can cause hyperglycaemia (HIP) during pregnancy, gestational diabetes mellitus (GDM) is still first detected during pregnancy [1]. HIP, whether diagnosed before, is dangerous and causes severe hyperglycaemia during pregnancy that persists after delivery. Gestational diabetes usually causes mild to moderate hyperglycaemia that also develops
in 50-60 % of women within 5 years of delivery. Because pregnancy occurs naturally, it can cause insulin resistance. The resulting hyperglycaemia in healthy women is compensated by pancreatic β-cell hyperplasia to meet the additional metabolism needs.
However, due to various genetic and environmental factors, GDM cannot be compensated, leading to hyperglycaemia [2]. Although GDM is associated with maternal-fetal complications, there are additional concerns. After giving birth, women with GDM are 10 times more likely to develop T2DM type 2 diabetes than women without GDM. Strict screening, monitoring, and preventive measures for women with postpartum GDM can help reduce T2DM in individual patients and even in the Population as a whole. Due to the rise in the current global prevalence of T2DM, the postpartum period of women with GDM is important in all countries, particularly those with a history of Gestational diabetes mellitus (GDM).
1Table 2 Global estimates of hyperglycaemia in pregnancy in 2021
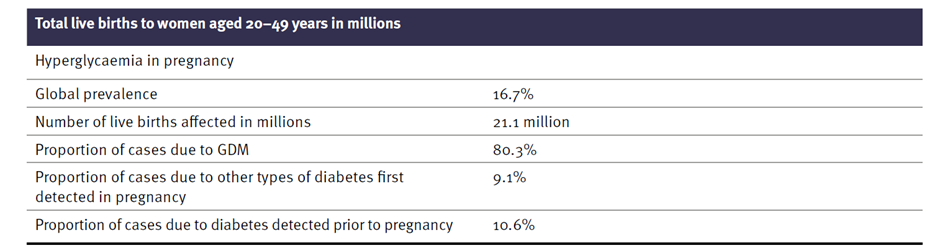
India is the largest country by Population and has the second-highest number of adults with T2DM globally. This number is expected to increase over 75% in the next 25 years [2].
2. Gestational Diabetes in South East Asia
Although T2DM has become a global epidemic [8], seven countries in Southeast Asia (India, Afghanistan, Bhutan, Maldives, Nepal, Pakistan, Sri Lanka, and Bangladesh) are the most severely affected by Diabetes and GDM. Disease severity accounts for approximately one-third of the global burden of diabetes and prediabetes [3]. In 2019, there were 88 million adults with diabetes in Southeast Asia, of whom more than half (57%) were undiagnosed [3]. If the current trend continues, 114 million Indians will be affected by 2045[2], and India may surpass China as the D.M. capital of the world.
Table 3: Hyperglycaemia in pregnancy (20–49 years) by IDF Region, ranked by 2021 age-adjusted
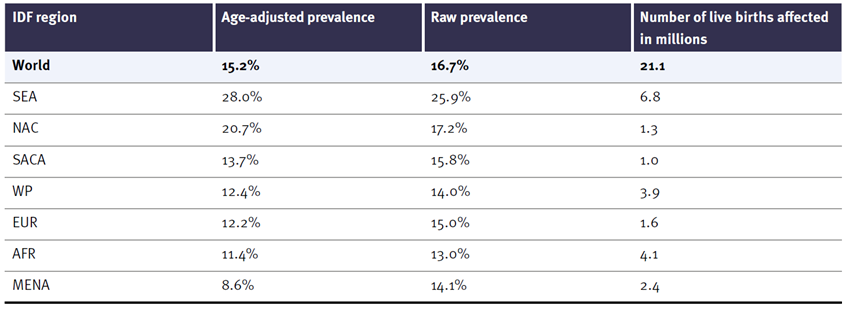
comparative prevalence estimates.
Estimates were available per IDF Atlas 2021 for seven IDF Southeast Asia (SEA) countries. All countries have relevant data except Bhutan for diabetes estimates in adults 20-79. Nine documents from six countries were used. Estimates for Bangladesh and Nepal are based on research over the past five years. The IDF estimates that the number of people with diabetes in Southeast Asia will increase by 68% to reach 152 million by 2045 [2].
Figure 2 Number and proportions of adults with undiagnosed diabetes Aged 20-79 years, per region, 2021
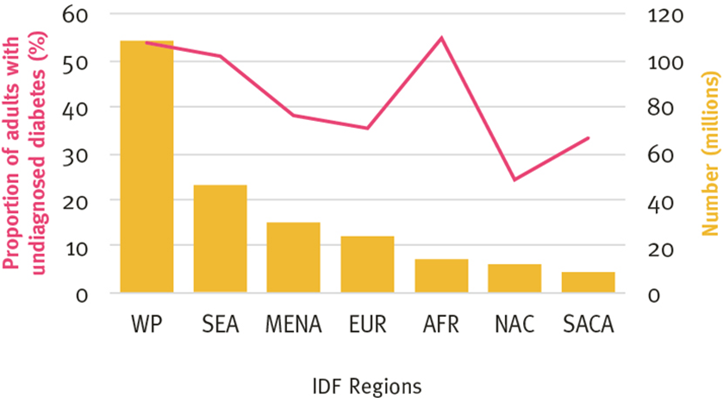
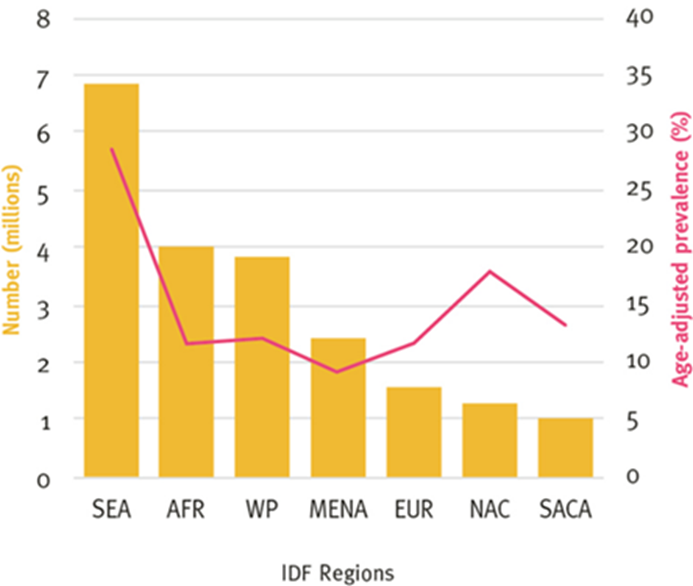
At the same time, the prevalence of diabetes will increase from 30% to 11.3%. The percentage of undiagnosed diabetes is 51.2%, the third highest in the IDF region (Fig 2, Fig 3). The proportion of pregnancies affected by hyperglycaemia is highest in the IDF region, at 25.9% (Fig 2, Fig 3).
Figure 3 Hyperglycemia in pregnancy Per IDF region,2021
A recent study involving 69 studies of 1,778,706 adults in India found that the prevalence of T2DM increased from 2.4% to 15% and from 3.3% in remote, urban, and rural areas of India between 1972 and 2019 showed an increase of 19.0% [4]. As the prevalence of GDM is similar to T2DM, an increase in blood sugar will change women affected by GDM.
Therefore, the prevalence of GDM in Asia is higher than in Europe because Asians have more T2DM. Recent epidemiological data suggest that T2DM affects young women developing HIP during pregnancy. If immediate action and measures are not taken, morbidity and mortality from D.M. and GDM will continue unabated. However, as women make up half the Population and GDM is a major cause of T2DM, managing GDM early in pregnancy and postpartum screening help prevent T2DM from rising.
3. India: An example of global GDM trends
Globally, approaches to GDM are diverse and confusing, with little consensus. In the United States, the 1979 National Diabetes Dataset Guidelines was one of the earliest efforts to conduct an objective, systematic study of D.M. and GDM. After this initial Guideline and four international workshops on GDM (1979-1997), the recommendations proposed significant changes in the screening and diagnosis of GDM. Over the next two years, (ACOG & ADA) the American College of Obstetricians and Gynaecologists and the American Diabetes Association (ACOG) followed this trend with new guidelines for GDM and HIP, Similar to the World Health Organization (WHO) 1980, 1985, 1999, and 2013. The Classification has also changed over time; Britain’s NICE National Institute for Health and Care Excellence, the Canadian Diabetes Association (CDA), and the Australian Gestational Diabetes Association (ADIPS) are some of the main standard-setting bodies (others) that use local and international research for updates. Therefore, over the past decade, due to international efforts, extensive research, and international consensus meetings, GDM treatment has seen an increase in screening, diagnosis, management, and postnatal care [5].
Thus, for example, separating GDM from DIP under the umbrella of HIP has clarified the meaning, and its relationship to HIP is now more clearly defined. In addition, the development and validation of diagnostic methods are very important as one universal Guideline. Countrywide is the need of time.
4. GDM prevalence in India
The prevalence of GDM in any given population depends on several factors, including characteristics of the study group: parental age, family history of diabetes, maternal weight and BMI, race, and ethnicity. Analysis of 84 studies showed that the combined prevalence of GDM in Asia was 11.5% (95% CI 10.9-12.0) [6]. However, there are significant differences in the majority of GDM due to differences in diagnostic criteria, screening methods, and work environments (e.g., urban and rural, home medical and community). Another study using data from 51 population studies found that the prevalence of GDM is affected by different diagnostic criteria.
In a study in the Indian Population using eight specialist diagnostic criteria for the same blood glucose results to diagnose OGTT, the prevalence of GDM ranged from 9.2% to 45.3%, depending on Therefore, most GDM in India ranges from 3.8% in Kashmir to 35% in Punjab [7].
Another review of 90 estimates from 64 studies showed that the prevalence of GDM in India ranged from 0% to 41.9%; the authors attribute this difference to different diagnosis models.
This study revealed large variations in the prevalence of GDM between regions. More importantly, the same standards were used (even in disease). The authors point out an important point: a different (other than “one size fits all”) approach will be costly in various parts of India.
5. Number of births with GDM in India
In India, 5-8 million women suffer from GDM each year [2]. India’s annual birth rate is about 25 million; this means that one-third of all babies will be affected by GDM. This information is based on the 2021 International Diabetes Federation (IDF) Atlas (10th edition), which states that 1 in 4 children born with HIP in Southeast Asia and 1 in 1 child worldwide has HIP [2]. In short, GDM is a bigger problem in India as it is more common.
Despite these challenges, it has encouraged Bangladesh, India, Pakistan, and Sri Lanka, the four largest countries responsible for more than 80 percent of the HIP burden live in Asia. With the help of policy experts, these schemes, federal and state grants, international organizations, and public health experts should conduct DIPSI tests on all pregnant women as blood sugar testing by hand using a glucometer is good today. Using a glucometer is common in Uttar Pradesh, Madya Pradesh, and other states under the National Health Mission funded program by Govt of India.
India faces a challenge for all countries with limited resources: how to apply the latest research within the constraints of personnel, laboratory equipment, and bureaucratic issues. There are also large cultural differences that create logistical problems. DIPSI screenings have the largest following in India and have been approved by the Govt of India MOHFW Guidelines 2014.
Because of differences in the prevalence of GDM in different states in India and given the country’s size, Experts agree that one method may not be suitable for all situations and that it is better to adapt to local solutions [1], a view shared by FIGO. The DIPSI test is still popular and accepted by major local organizations. So far, this is good practice.
With the high prevalence of Type 2 diabetes, there has been an increase in the incidence of GDM in India over the past two decades, mainly due to rapid changes in lifestyle, socioeconomics, and epigenetics that increase the prevalence of the disease. Indian women are estimated to have an 11 times higher risk of establishing GDM compared to women of other races and ethnicities. A 4 to 4 prevalence of GDM has been reported in India, 6% to 14% in urban parts of India and 1.7% to 13.2% in rural India. Overall, the incidence is between 3.8% and 17%. The majority in different parts of India is 9%, ranging from 35% in states like Punjab [2] to 17.9% in southern states like Tamil Nadu. [3] A lower rate of GDM (3.8%) has been reported in some regions, such as Kashmir. [4] A community study by Seshiah V et al. in South India showed that GDM prevalence in urban areas was 17%.8% compared to 9.9% in rural areas and 13.7%, similar to the population-based study with NHM in Uttar Pradesh [5]. Some diagnoses to arrive at GDM diagnosis for future diabetes prevention in India suggested. The Gestational Diabetes Working Group of India (DIPSI) [6] supports “one step” for the diagnosis of GDM, which is recommended by the NHM guidelines, GOI [7] for GDM (with or without fasting OGTT).
There are many reviews for all pregnant women. The onset of GDM in pregnant women can be delayed and is called true GDM. Many studies have been published to explain overt or true GDM formation. The severity of true GDM represents only the tip of the GDM disease iceberg. However, there are many cases of latent gestational diabetes (PGDM) in the Population resulting from Type-1DM or Type 2 diabetes before pregnancy. Although the prevalence of PGDM in India is low, due to the long duration of hyperglycaemia and its impact on children’s health, these women are at high risk for many complications, such as macrosomia, neonatal diabetes, and polyhydramnios. A study by Fang W et al. shows that the prevalence of PGDM is 0.66%. This proportion of Asians [7] is lower than for other races. However, these women often suffer from many diseases, such as thyroid disease, high blood pressure, and pyelonephritis, that cause fertility problems.
Summary:
India demonstrates tremendous progress worldwide in achieving HIP pregnancy Screening by “Universal Single Test Procedure” advocated by DIPSI and adopted by Govt of India, MOHFW 2014 Guidelines [8].
The importance of GDM management is simple; If diagnosed, treated, and followed up after birth, it will reduce the burden of T2DM in a country now and in future generations. Therefore, GDM monitoring has the potential to change future predictions regarding T2DM.
Specifically, 90% of HIP births occur in low- and middle-income countries. There are significant challenges in universal screening for GDM, with coverage rates ranging from 10% to 90%. Missing out or not treating women with GDM leads to short-term and long-term complications associated with GDM.
India faces a challenge for all countries with limited resources: how to apply the latest research within the constraints of personnel, laboratory equipment, and bureaucratic issues. There are also large cultural differences that create logistical problems. DIPSI screenings have the largest following in India and are also approved by Govt of India MOHFW Guidelines 2014.
Because of differences in the prevalence of GDM in different states in India and given the size of the country, Experts agree that one method may not be suitable for all situations and that it is better to adapt to local solutions [8], a view shared by FIGO. The DIPSI test is still popular and accepted by major local organizations. So far, this is good practice.
New WHO recommendations and coverage targets for Diabetes
On January 26 and 27, the 150th session of the WHO Executive Board issued a report by the DG Director General on the political declaration of the third high-level meeting of the General Assembly on preventing and controlling Non-communicable Conditions[9]
The document recommendations for MS Member Nations States, international Collaborators, and WHO to strengthen and monitor diabetes responses within national NCD programs by enhancing national capacity, lowering prevention of risk factors, strengthening health systems through PHCs healthcare and Universal health coverage UHC, supporting high-quality new research, and monitoring, control trends, determinants.
The Documents also cover a proposed set of diabetes people coverage Goals to be achieved by 2030:
80% of the population living with Diabetes is diagnosed
80% of the population with screened, diagnosed Diabetes have fairly good control of glycemia
80% of the population with screened, diagnosed Diabetes have fairly good control of BP
60% of the population over >40 years with Diabetes receive lipid-lowering drugs
100% of the population with type 1 diabetes have access to affordable insulin management and blood glucose self-monitoring
While these targets are not flawless, and the IDF would have liked to see a target of 100% diagnosis of children living with type 1 diabetes, we believe they provide a very strong direction for Member Nations States to act on Diabetes in the present decade by a core area of the WHO Global Diabetes Compact [9,10,11]
References:
1.International Diabetes Federation.IDF Diabetes Atlas, 10th ed. Brussels, Belgium: International Diabetes Federation, 2021. Available at: https://www.diabetesatlas.org
2. Mantri, N., Goel, A.D., Patel, M. et al. National and regional prevalence of gestational diabetes mellitus in India: a systematic review and Meta-analysis. BMC Public Health 24, 527 (2024). https://doi.org/10.1186/s12889-024-18024-9
3. Seshiah V, Balaji V, Balaji MS, Sanjeevi CB, Green A. Gestational diabetes mellitus in India. J Assoc Physicians India. 2004; 52: 707-11.
4. Raja MW, Baba TA, Hanga AJ, Bilquees S, Rasheed S, Haq IU et al. A study to estimate the prevalence of gestational diabetes mellites in an urban block of Kashmir valley (North India). Int J Med Sci Public Health. 2014; 3(2): 191-195
5. Jain R, Davey S, Arya S, Davey A, Raghav SK. A prospective study with outcome on gestational diabetes mellitus. J Evol Med Dent Sci. 2015; 4: 15640‑7.
6. Seshiah V, Das AK, Balaji V, Joshi SR, Parikh MN, Gupta S; Diabetes in Pregnancy Study Group. Gestational diabetes mellitus–guidelines. J Assoc Physicians India. 2006; 54: 622-8.
7. Fong A, SerraA, Herrero T, Pan D, Dotun Ogunyemi. Pre-gestational versus gestational diabetes: a population-based study on clinical and demographic differences. J Diabetes complications. 2014; 28(1): 29-34.
8.Diagnosis and Management of Gestational Diabetes Mellitus. Available online: https://nhm.gov.in/New_Updates_2018/NHM_Components/RMNCH_MH_Guidelines/Gestational-Diabetes-Mellitus.pdf (accessed on 15 March 2021).
9.Resolutions and Decisions, Annexes (WHA42/1989/REC/1). 4 Ibid., Fifty-seventh World Health Assembly, Geneva, 17–22 May 2004, Resolutions and Decisions, Annexes (WHA57/2004/REC/1).
10.World Health Assembly, 57. (2004). Fifty-seventh World Health Assembly, Geneva, 17-22 May 2004: resolutions and decisions, annexes. World Health Organization. https://iris.who.int/handle/10665/20159
11.Report of the first meeting of the WHO Global Diabetes Compact Forum: virtual meeting, 10‑11 November 2021. Geneva: World Health Organization; 2022. License: CC BY-NC-SA 3.0 IGO. 9789240045705-eng.pdf
- Acknowledgment
Not applicable
- Funding
Not applicable
- Informed Consent
Not applicable
- Conflict of Interest Statement
All the authors declared “No Conflict of Interest” with this publication.
The article is Open Access and are licensed under a Creative Commons Attribution 4.0 International License, visit http://creativecommons.org/licenses/by/4.0/
- DOI: 10.62996/daj.30122024
- Cite this Article
Rajesh Jain1, Veeraswamy Seshiah2. Global Picture of Diabetes & GDM. Diabetes Asia Journal.2024; 1(3):01-10. https://doi.org/10.62996/daj.30122024

