Research Article
Siyamak Jalal Hosseini1*, Soheil Mansourian2, Mohammadreza Shoghli3, Hermon Eyob Fesseha4 , Rajesh Jain5
Submitted: 14 June 2024;
Accepted: 10 July 2024; Published: 27 June 2024
1. Assistant Professor, Tehran University of Medical Sciences, Tehran, Iran; 2. Professor Tehran University of Medical Sciences, Tehran, Iran; 3. Doctoral Researchers, Department of Population Health, University of Helsinki, Helsinki, Finland; 4. Hermon Eyob Fesseha: MD, cardiology resident, Peijas Hospital District of Helsinki and Uusimaa (HUS), University of Eastern Finland, University of Helsinki, Helsinki, Finland; 5. Consultant Diabetes, Jain hospital & research Centre, Kanpur, India.
Corresponding Author:1* Assistant Professor, Tehran University of Medical Sciences, Tehran, Iran. email [email protected]
Abstract: This study examined 204 patients undergoing CABG surgery at Tehran Heart Center between Ordibehesht 1402 and Ordibehesht 1403 for postoperative complications.
Objective: Investigation and Comparison of Complications in Single-Wire and Double-Wire Sternal Closure Methods Following Open Heart Surgery in Patients Referred to Tehran Heart Center from May 2023 to May 2024
Methods: Patients were divided into two groups of 102 each, with Group 1 undergoing sternal closure using a single-wire method and Group 2 using a double-wire method.
Results: All patients were discharged after surgery and followed up for one year. The age range was 44 to 75, with 21 patients aged 45-55 (10%), 133 patients aged 55-65 (65%), and 50 patients aged 65-75 (24%). Both groups had similar age distributions. Of the total patients, 78 were female (38.2%) and 126 were male (61.8%), indicating a higher prevalence of cardiovascular disease in males.
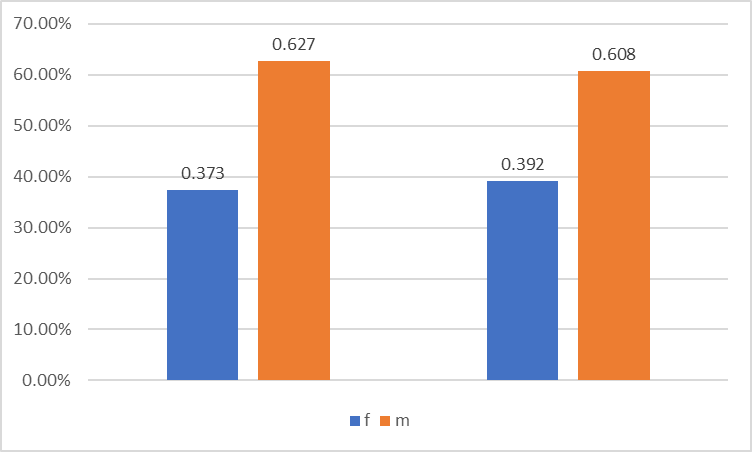
In Group 1, 37% were women and 63% were men; in Group 2, 39% were women and 61% were men. We compared four parameters between the two groups: infection, pain, stability, and tissue reaction.
In Group 1, 8 patients (7%) developed superficial skin infections, with a readmission rate of 1%. In Group 2, 6 patients (5%) developed superficial infections, with one readmission. Statistical analysis showed no significant difference in infection rates between the two methods.
Regarding pain after surgery, 17 patients in Group 1 (10%) reported postoperative pain, which decreased to 2% after three months and disappeared completely after one year. In Group 2, 24 patients experienced pain, which also resolved within a year. However, statistical analysis revealed a significant difference in pain rates between the two groups, indicating more pain in patients with double-wire closure.
Conclusion:
The two groups had no significant differences in stability and tissue reaction. Our study suggests that the single-wire closure method may lead to less postoperative pain in stable patients without risk factors, contributing to earlier recovery and improved quality of life.
Methodology and Procedure:
We conducted a comparative study on sternal closure methods following CABG surgery among patients treated at the Tehran Heart Center between 2022 and 2024.
We divided all patients into two groups, each consisting of 102 individuals. Gender distribution and age demographics were carefully balanced between the groups to prevent selection bias. Patients with poorly controlled metabolic diseases were excluded from the study. Group 1 underwent sternal closure using a single-wire method, while Group 2 underwent closure with double wires.
After performing surgeries on all 204 patients, they were discharged from the hospital and followed up for one-year post-surgery. The age range of the patients was from 44 to 75, with 21 patients aged 45-55 (10%), 133 patients aged 55-65 (65%), and 50 patients aged 65-75 (24%). Both groups had similar age distributions. Of the total, 78 patients were women, and 126 were men, consistent with the documented higher prevalence of cardiovascular disease in men.
Group 1 comprised 37% women and 63% men, while Group 2 had 39% women and 61% men. We analyzed four parameters across both groups: infection, pain, stability, and tissue reaction. In Group 1, 8 patients (7%) developed infections from sternotomy, with one patient requiring readmission. Similarly, in Group 2, 6 patients developed infections, with one readmission. Statistical analysis using SPSS showed no significant difference in infection rates between the two closure methods.
Both groups showed similar stability and tissue reaction outcomes, with no dehiscence or adverse tissue reactions observed. A sternal dehiscence is a catastrophic event in cardiac surgery. Both sternal closure methods yielded comparable outcomes in stable patients without risk factors. However, the double-wire method required a longer operation than the single-wire method.
In the assessment of post-CABG pain, remarkable findings emerged. In Group 1, 44 patients experienced pain, with 32 having mild pain, 10 moderate pain, and 2 severe pain. In contrast, Group 2 had 55 patients reporting pain, with 40 experiencing mild pain, 11 moderate pain, and 4 severe pain. After three months, only one patient in Group 1 continued to experience pain, which resolved by the sixth month. Conversely, all patients in Group 2 were pain-free after six months.
Statistical analysis revealed that 43% of patients in Group 1 experienced pain compared to 53% in Group 2. Based on these findings, we concluded that avoiding double-wire sternal closure in stable patients (those without poorly controlled metabolic conditions, risk factors, sepsis, or osteopenia) could enhance the quality of life and rehabilitation outcomes following CABG surgery.
Introduction
Currently, most heart surgeries are performed via midline sternotomy. This type of incision was first proposed in 1857 and gained popularity in 1957. Generally, sternotomy complications are rare; however, they are usually serious when they occur. The most common complications include infection and mediastinitis [1]. Sternotomy is a surgical procedure in which surgeons
make a vertical incision along the midline of the chest. This approach replaced the previous bilateral thoracotomy method. Sternotomy became popular mainly because it is less painful than previous models, and it quickly became apparent that it could lead to problems such as infection or wound dehiscence [1]. Sternotomy is a surgical procedure in which the surgeon creates an internal vertical incision along the midline of the chest. This allows access to the entire chest area, including the heart and lungs [2]. This approach has several advantages, including less pain, better access to pleural cavities, and greater protection of chest muscles [7]. Overall, sternotomy is a relatively safe method; however, it may sometimes lead to complications [2]. One of the most common complications is infection, although it affects only about 3% of patients [1]. In this regard, infection can be superficial or serious; however, the results of both can be severe (5). They usually lead to hospitalization and may threaten life. Between 4 and 47% of patients who develop sternotomy infections lose their lives [2]. Usually, infections result from sternal osteomyelitis or mediastinitis; these complications usually occur between 7 and 12 days after surgery [1]. However, in most patients, it progresses in the first week after surgery, mediastinitis is the most serious and problematic complication, mediastinitis is caused by infection and is very serious and sometimes fatal. This usually requires treatment (2). Sternal infections associated with sternotomy are related to three factors [3]. The first group consists of the patient’s intrinsic factors before surgery. However, the second group consists of developing the surgical method [3]. Finally, the third and final group consists of postoperative factors.
Pre-operative Factors
In this regard, risk factors include being female, elderly, having diabetes, chronic respiratory infections, kidney failure, or smoking [3].
Surgical Factors
These include urgency of intervention, duration of intervention, type of intervention, excessive electrocautery, and cardiogenic shock [3].
Post-operative Factors
These include prolonged mechanical ventilation, bleeding, and the use of inotropes. When pre-existing risk factors are identified, recovery is usually successful. This can reduce the risk of complications and make them easier to manage. Obesity, diabetes, and aging are factors that deserve special attention, and usually, infection treatment includes irrigation, negative pressure wound therapy, debridement
surgery, wound coverage, and systemic antibiotic use [1-3].
Postoperative care
includes gently cleaning the wound with mild soap and carefully drying it [4]. The stitches are removed after 2 weeks, and wound closure tapes, which facilitate their healing, are removed or fall off
after one week [4]. It is normal for patients to experience occasional and recurrent pain; if they feel it, they should take pain relievers. It is also normal for their incision to be slightly
swollen, and after a few months, everything should return to normal [1]. The cause of chest pain after open heart surgery includes Musculoskeletal reasons (the most common cause) [7]. Myocardial ischemia (reduced blood and oxygen supply to the heart) [7] Pericarditis (such as Dressler’s syndrome) [7].
The good news is that chest pain after heart surgery is not always an indication of imminent danger. Depending on the type of surgery you have, this pain can even be considered a
permanent part of the recovery period (especially for chest surgeries). Additionally, chest pain can result from heartburn [3]. After heart surgery, the patient needs a precise regular diet plan, a suitable exercise program, and engaging in activities appropriate to their condition [6]. As mentioned, CABG surgery aims to improve quality of life and enhance individuals’ quality of life [6]. Therefore, efforts should be made to impose the least burden on the patient. In this project, our goal is to investigate the methods of sternal closure to reduce the incidence of infection and sternal dehiscence and to speed up the patient’s return to the community by reducing the complications and the cost of re-treatment for the patient. In this project, we focus on patients’ complications, pain, and infections after sternal closure using single-wire and double-wire methods. Post-operative complications are divided into two groups: high-risk and low-risk.
The first group includes death, cardiac arrest, stroke, acute bleeding, platelet drop, etc. The second group comprises sternal wound infection, sternal instability, and post-operative pain. Complications in the first group are unrelated to the type of sternal closure method, but in the second group, controlling factors can reduce low-risk complications.
General Objective: To investigate post-operative complications and compare single-wire and double-wire sternal closure methods after open-heart surgery.
Specific Objectives:
-
- Compare the incidence of post-operative infection in both methods.
-
- Assess sternal stability.
-
- Evaluate the speed of patients’ return to daily activities.
-
- Investigate the level of post-operative chest pain in both methods.
-
- Examine the demographic age of patients undergoing open-heart surgery.
-
- Determine the best method for sternal closure.
-
- Prevent patient rehospitalization.
-
- Reduce additional costs for patients and hospitals.
-
- Improve the quality of life for patients.
Hypotheses or Research Questions:
Literature review
Julian Lozanov et al. (2008): This study compared the complications of double sternal wire closure versus single wire closure. It involved 75 patients in each group and found that while stability was higher in the first method, the difference was not statistically significant. The infection rate was similar in both methods.
Double Crisscross Sternal Wiring Study (2003): This Italian study included 350 patients in each group. The double wire method was recommended due to lower infection rates (1% vs. 6%) and decreased sternal dehiscence (2% vs. 8%). However, post-operative pain levels were similar in both methods.
University of Michigan Study (2004): This study found no significant difference between the two sternal closure methods regarding stability and infection rate. Although the double-wire group had slightly more pain, it wasn’t statistically significant. Each group consisted of 100 patients.
German Study (2008): In this study, with 105 participants in each group, there was no significant difference in initial infection rates between the two closure methods. However, double wire closure showed better results in delayed infection and dehiscence. This study mainly focused on low-risk patients.
Barts Heart Center London Study (2020): This study involved 120 participants in each group. A higher rate of sternal instability was noted in the single-wire group than in the double-wire closure group. The stability was significantly higher in the double-wire group. Both initial and delayed infection rates were not significantly different, but sternal dehiscence was notably lower in the double-wire group (5 cases compared to 19 in the single-wire group).
Materials and Methods
-
- Study Type: Epidemiological Analytical (Case-Control, Cohort)
Execution Method and Research Design:
Execution Method: (Considering the previous section, describe the necessary items for each type of study here.) Study Population: Our population consists of patients undergoing open-heart surgery at Tehran Heart Center from Ordibehesht 1402 to Ordibehesht 1403. These patients are divided into two groups, with 102 individuals in each group. The first group undergoes single-wire closure, and the second group undergoes double-wire sternum closure. Patients with immune deficiencies or unstable conditions are excluded from the study. Patient selection is randomized, and both groups are matched for medical conditions.
Data Collection Tool Specifications and Collection Method: Our study collects data from patients undergoing open-heart surgery at Tehran Heart Center from Ordibehesht 1402 to Ordibehesht 1403. These patients are divided into two groups, with 102 individuals in each group. The first group undergoes single-wire closure of the sternum, and the second group undergoes double-wire closure of the sternum. Information is recorded through follow-up, examination, and questionnaires during subsequent clinic visits.
Sample Size Calculation Method, Number of Samples: To calculate the minimum required sample size, the main variable in the current study, which is comparing post-operative infections in two methods of sternum closure (single wire vs. double wire), is considered. Based on the survey by Kiessling AH et al., which reported the prevalence of post-operative infections as p_1=6/50 for single wire and p_2=1/50 for double wire closure, with a Type I error of α=0.05 and a power (1-β)=0.80, G*Power software is utilized. The minimum required sample size is calculated using the independent proportions test, resulting in 102 individuals in each group. In other words, this study’s minimum required sample size is 204 individuals, as detailed below.
Study Reference:
-
- Chow SC. Sample size calculations for clinical trials. Wiley interdisciplinary reviews: Computational statistics. 2011 Sep;3(5):414-27.
-
- Kiessling AH, Isgro F, Weisse U, Möltner A, Saggau W, Boldt J. Advanced sternal closure to prevent dehiscence in obese patients. The Annals of Thoracic Surgery. 2005 Oct 1;80(4):1537-9.
Analysis:
-
- Test Type: z tests – Proportions: Difference between two independent proportions
-
- Analysis Approach: A priori: Compute required sample size
-
- Input Parameters:
-
- Tail(s): Two
-
- Proportion p1: 0.02
-
- Proportion p2: 0.12
-
- α error prob: 0.05
-
- Power (1-β error prob): 0.8
-
- Allocation ratio N2/N1: 1
-
- Input Parameters:
-
- Output:
-
- Critical z: 1.9599640
-
- Sample size group 1: 102
-
- Sample size group 2: 102
-
- Total sample size: 204
-
- Actual power: 0.8038831
-
- Output:
Data Analysis Methodology:
In the present study, absolute and relative frequency distributions for qualitative variables and the mean and standard deviation for quantitative variables have been reported for descriptive data analysis. Moreover, for inferential data analysis, the Shapiro-Wilk test has been used to assess the normality of the data, the independent t-test (or non-parametric Mann-Whitney test) for comparing quantitative variables in two methods of sternal closure (single wire vs. double wire), and Chi-square test for comparing post-operative complications (measured on a qualitative scale) in the two study methods. Additionally, the collected data will be analyzed using SPSS version 28 software. Finally, a significance level of 0.05 (P < 0.05) has been considered for all analyses.
Ethical Considerations: Preserving the anonymity and confidentiality of individuals’ names and identities is a priority in all stages of this research project.
Implementation Constraints and Methods of Mitigation:
-
- The study population may not represent the general population since the patients are hospitalized in the Heart Center Hospital.
Mitigation: Although the study population may not fully represent the general population, efforts can be made to ensure that the sample is diverse and includes patients with various demographic characteristics and medical conditions.
-
- Inaccurate follow-up after surgery.
Mitigation: Implement strategies to improve patient follow-up, such as providing clear instructions regarding post-operative care and scheduling regular follow-up appointments with healthcare providers.
-
- Poor patient cooperation in post-operative care.
Mitigation: Offer education and support to patients to enhance their understanding of the importance of post-operative care and encourage them to actively participate in their recovery process. Provide resources and assistance as needed to address any barriers to cooperation.
Ethical Considerations (Ethical Review) (According to Ethical Standards and Guidelines of the Relevant Ministry):
Adherence to the principles of the Helsinki Declaration in ethical considerations. Maintaining patient confidentiality and privacy. Avoiding judgment of patients’ conditions. Respecting the dignity and rights of patients.
Results
Frequency of Gender in Two Studied Groups
In the first group, out of 102 individuals, 38 were female (37.3%) and 64 were male (62.7%). In the second group, out of 102 individuals, 40 were female (39.2%) and 62 were male (60.8%). Out of 204 individuals, 78 were female, and 126 were male. Based on the chi-square analysis, the gender distribution in the two groups is equal (P=0.773).
|
Table 1 : Frequency of Gender in Two Studied Groups |
|||||||
|
|
Group 1 |
Group 2 |
Total |
||||
|
sex |
f |
Count |
38 |
40 |
78 |
||
|
Percent |
37.3% |
39.2% |
38.2% |
||||
|
m |
Count |
64 |
62 |
126 |
|||
|
Percent |
62.7% |
60.8% |
61.8% |
||||
|
Total |
Count |
102 |
102 |
204 |
|||
|
Percent |
100.0% |
100.0% |
100.0% |
||||
|
Chi-Square Tests |
|||||
|
|
Value |
df |
Asymptotic Significance (2-sided) |
Exact Sig. (2-sided) |
Exact Sig. (1-sided) |
|
Pearson Chi-Square |
.083a |
1 |
.773 |
|
|
|
Continuity Correctionb |
.021 |
1 |
.885 |
|
|
|
Likelihood Ratio |
.083 |
1 |
.773 |
|
|
|
Fisher’s Exact Test |
|
|
|
.886 |
.443 |
|
Linear-by-Linear |
.083 |
1 |
.774 |
|
|
|
N of Valid Cases |
204 |
|
|
|
|
|
a. |
|||||
|
b. |
|||||
Frequency of Post-Operative Infection in Two Studied Groups
In the first group, out of 102 individuals, 94 (92.2%) did not have a post-operative infection, and 8 (7.8%) had an infection. In the second group, out of 102 individuals, 96 (94.1%) did not have a post-operative infection, and 6 (5.9%) had an infection. Out of 204 individuals, 190 did not have a post-operative infection, and 14 had an infection. Based on the chi-square analysis, there is no significant difference in the incidence of postoperative infection.
|
Table 2: Frequency of Post-Operative Infection in Two Studied Groups |
|||||
|
|
Group 1 |
Group 2 |
Total |
||
|
Infections after |
No |
Count |
94 |
96 |
190 |
|
Percent |
92.2 % |
94.1 % |
93.1 % |
||
|
Yes |
Count |
8 |
6 |
14 |
|
|
Percent |
7.8 % |
5.9 % |
6.9 % |
||
|
Total |
Count |
102 |
102 |
204 |
|
|
Percent |
100.0 % |
100.0 % |
100.0 % |
||
|
Chi-Square Tests |
|||||
|
|
Value |
df |
Asymptotic Significance (2-sided) |
Exact Sig. (2-sided) |
Exact Sig. (1sided) |
|
Pearson Chi-Square |
.307a |
1 |
.580 |
|
|
|
Continuity Correctionb |
.077 |
1 |
.782 |
|
|
|
Likelihood Ratio |
.308 |
1 |
.579 |
|
|
|
Fisher’s Exact Test |
|
|
|
.783 |
.391 |
|
Linear-by-Linear |
.305 |
1 |
.581 |
|
|
|
N of Valid Cases |
204 |
|
|
|
|
|
a. |
|||||
|
b. |
|||||
Group 1:
-
- No Pain: 58 (56.9%)
-
- Mild Pain: 32 (31.4%)
-
- Moderate Pain: 10 (9.8%)
-
- Severe Pain: 2 (2.0%)
Group 2:
-
- No Pain: 47 (46.1%)
-
- Mild Pain: 40 (39.2%)
-
- Moderate Pain: 11 (10.8%)
-
- Severe Pain: 4 (3.9%)
Overall, out of 204 individuals:
-
- No Pain: 105 (51.5%)
-
- Mild Pain: 72 (35.3%)
-
- Moderate Pain: 21 (10.3%)
-
- Severe Pain: 6 (2.9%)
The chi-square test indicates a significant difference between the two groups regarding pain incidence (P<0.05).
|
Table 3 : Frequency of Pain in Two Studied Groups |
|||||
|
|
Group |
Group 2 |
Total |
||
|
pain |
No Pain |
Count |
58 |
47 |
105 |
|
Percent |
56.9% |
46.1% |
51.5% |
||
|
Mild Pain |
Count |
32 |
40 |
72 |
|
|
Percent |
31.4% |
39.2% |
35.3% |
||
|
Moderate Pain |
Count |
10 |
11 |
21 |
|
|
Percent |
9.8% |
10.8% |
10.3% |
||
|
Severe Pain |
Count |
2 |
4 |
6 |
|
|
Percent |
2.0% |
3.9% |
2.9% |
||
|
Total |
Count |
102 |
102 |
204 |
|
|
Percent |
100.0% |
100.0% |
100.0% |
||
|
Chi-Square Tests |
|||
|
|
Value |
df |
Asymptotic Significance (2-sided) |
|
Pearson Chi-Square |
2.756a |
3 |
.431 |
|
Likelihood Ratio |
2.772 |
3 |
.428 |
|
Linear-by-Linear |
2.045 |
1 |
.153 |
|
N of Valid Cases |
204 |
|
|
|
a. |
|||
Discussion
This study evaluated 204 patients undergoing CABG surgery at Tehran Heart Center from Ordibehesht 1402 to Ordibehesht 1403 for post-operative complications. Patients were divided into two groups of 102 individuals, with one group undergoing single-wire closure and the other undergoing double-wire sternal closure. Patients with risk factors such as osteopenia and corticosteroid use, poor coronary status, and end-stage disease were excluded from the study. The age range of the population in the study was between 45 and 75 years, with 10% of the population in the age group (45-55), 65% in the age group (55-65), and 24% in the age group (65-75). The distribution of age groups was equal in both groups.
Of the total 204 individuals, 78 were female (38.2%) and 126 were male (61.8%), indicating a higher prevalence of coronary artery disease in males. The distribution of females was 37% in group 1 and 39% in group 2. According to previous studies, the prevalence of coronary artery disease is higher in males. Regarding post-operative infection, 7% of individuals in group 1 and 5% in group 2 had superficial skin infections, with a readmission rate of 1% and 1 individual in group 1 and 5% and 1 individual in group 2. Statistically, this difference was insignificant, indicating no difference in infection between the two methods. Studies in Italy, the US, and Qatar have shown no difference in infection rates between single-wire and double-wire methods, with consistent results.
In terms of post-operative pain, 43 of the individuals in group 1 experienced pain after surgery, with 32 having mild pain, 10 moderate pain, and 1 severe pain, which resolved in all patients after 3 months. In group 2, 57 experienced pain in group 2, 42 had mild pain, 11 had moderate pain, and 4 had severe pain, with only 4 individuals experiencing pain at the 3-month follow-up, but they did not complain of pain at the 3-month visit. Statistically, the difference between 42.2% and 55.9% was significant, indicating more pain in patients with double-wire closure post-operation. According to studies, post-operative pain is higher in the double-wire group, while in Italy and Qatar, pain is similar in both groups.
There was no significant difference in appearance, stability, and tissue reaction between the two groups, indicating similarity between the two methods. Considering this study, the prevalence of coronary artery disease is higher in males. The incidence of infection was higher in group 1, but statistically, there was no difference. There was more pain in the double-wire group, and patients required more pain medication. With consistent results and stability in both methods, performing single-wire closure can prevent additional pain in patients without risk factors, allowing them to return to normal sooner.
References
-
- Stephenson LW. Historical perspective of The American Association for Thoracic Surgery: John W. Kirklin, MD (1917-2004). J Thorac Cardiovasc Surg. 2007 Jul;134(1):225-8. doi: 10.1016/j.jtcvs.2007.02.032
-
- Trumble DR, McGregor WE, Magovern JA. Validation of a bone analog model for studies of sternal closure. Ann Thorac Surg. 2002 Sep;74(3):739-44; discussion 745. doi: 10.1016/s0003-4975(02)03699-8
-
- Losanoff JE, Jones JW, Richman BW. Primary closure of median sternotomy: techniques and principles. Cardiovasc Surg. 2002 Apr;10(2):102-10. doi: 10.1016/s0967-2109(01)00128-4
-
- Cimochowski GE, Harostock MD, Brown R, Bernardi M, Alonzo N, Coyle K. Intranasal mupirocin reduces sternal wound infection after open heart surgery in diabetics and nondiabetics. Ann Thorac Surg. 2001 May;71(5):1572-8; discussion 1578-9. doi: 10.1016/s0003-4975(01)02519-x
-
- McGregor WE, Payne M, Trumble DR, Farkas KM, Magovern JA. Improvement of sternal closure stability with reinforced steel wires. Ann Thorac Surg. 2003 Nov;76(5):1631-4. doi: 10.1016/s0003-4975(03)00760-4.
-
- Balachandran S, Lee A, Denehy L, Lin KY, Royse A, Royse C, El-Ansary D. Risk Factors for Sternal Complications After Cardiac Operations: A Systematic Review. Ann Thorac Surg. 2016 Dec;102(6):2109-2117. doi: 10.1016/j.athoracsur.2016.05.047
-
- Cataneo DC, Dos Reis TA, Felisberto G, Rodrigues OR, Cataneo AJM. New sternal closure methods versus the standard closure method: systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2019 Mar 1;28(3):432-440. doi: 10.1093/icvts/ivy281
-
- Losanoff JE, Basson MD, Gruber SA, Huff H, Hsieh FH. Single wire versus double wire loops for median sternotomy closure: an experimental biomechanical study using a human cadaveric model. Ann Thorac Surg. 2007 Oct;84(4):1288-93. doi: 10.1016/j.athoracsur.2007.05.023
Supplementary
Table 1 Pain and Infection in Single-Wire and Double-Wire Sternal Closure Methods Following Open Heart Surgery
| N = 102 Post-Cardiac surgery (Mean ± SD) No (%) Single wire closure | N = 102 Post-Cardiac Surgery (Mean ±S D) No (%) Double wire closure | P-value | |
| Age (years) | 24.0 ± 4.5 | 24.6 ± 4.7 47 | 0.961 |
| Female | 38 (37.3%) | 40 (39.2%) | 0.773 |
| Male | 64 (62.7%) | 62 (60.8%) | 0.773 |
| Post-operative pain | 43(42.2) | 57(55.9) | 0.049 |
| No Pain | 58 (56.9%) | 45 (44.1%) | 0.123 |
| Mild Pain | 32 (31.4%) | 42(41.2%) | 0.241 |
| Moderate Pain | 10 (9.8%) | 11 (10.8%) | 0.818 |
| Severe Pain | 1 (0.98) | 4 (3.9%) | 0.407 |
| Post-operative Infection | 8 (7.8%) | 6 (5.9%) | 0.580 |
| No Infection | 94 (92.2%) | 96 (94.1%) | 0.580 |
| Skin superficial Infection | 7(6.9) | 6 (5.9) | |
| Multi | 51(54.9) | 68 (54.4) | |
-
- Acknowledgment
Not applicable
-
- Funding
Not applicable
-
- Informed Consent
Not applicable
-
- Conflict of Interest Statement
All the authors declared “No Conflict of Interest” with this publication.
-
- Additional Information
Not applicable
This open-access article is distributed under the terms of the Creative Commons Attribution License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
-
- DOI: 10.62996/daj.05072024
Cite this Article: Siyamak Jalal Hosseini1*, Soheil Mansourian2, Mohammadreza Shoghli3, Hermon Eyob Fesseha4, Rajesh Jain5. Comparative Analysis of Sternal Closure Methods Following CABG Surgery: A Study from the Tehran Heart Center. Diabetes Asia Journal. 2024;1(1):28-40. 10.62996/daj.05072024


