Rajesh Jain1*, Veeraswamy Seshiah2 N, Guneeta Mehta Jain3, Pikee Saxena4, 5Shaily Agarwal, 6Sadhana Tiwari
2MD, FRCP, Distinguished Professor, The Tamil Nadu Dr. M.G.R. Medical University, Chennai, India;3MD, Department of Obstetrics & Gynecology, Med Gynae clinic, Saharanpur, UP, India; 4MD, Department of Obstetrics and Gynecology, Lady Hardinge Medical college, New Delhi; 5MD, Department of Obstetrics & Gynecology, GSVM Medical College, Kanpur, India; 6MD Fellow, Department of Obstetrics and Gynecology, GSVM Medical College, Kanpur, India
Submitted: 28 June 2024; Accepted: 10 July 2024; Published: 20July 2024
1*Corresponding Author, Rajesh Jain MD, PG Diploma Diabetes (UK), Project Manager, Diabetes Prevention Control Project, NHM, Uttar Pradesh, India, 108 B Gandhi gram, Vinobha Nagar, Kanpur-208007, India Email: Email: Email:[email protected]
Abstract
Gestational diabetes mellitus (GDM) is a metabolic disorder caused by carbohydrate intolerance during pregnancy for the first time. This disease is very important as it affects the mother and fetus. It is said that GDM disrupts the pregnancy process and causes many diseases, such as recurrent miscarriage, congenital anomalies, preeclampsia, stillbirth, macrosomia, preterm birth, and emergency delivery after pregnancy, pregnancy, and delivery. It also causes long-term complications by inducing type 2 diabetes mellitus in mothers and children. GDM is generally considered a lifestyle disorder, and therefore, its burden varies by race, geographic boundaries, genetics, and reproductive risk.
Consequently, it is necessary to investigate the prevalence and risk of GDM to evaluate prevention strategies. The first trimester early management of Dysglycemia with Medical Nutrition Treatment (MNT) and Metformin is promising. It might be advocated in the future for curtailing the epidemic of GDM and Type 2 Diabetes.
Recently, the TOBOGM study and our ongoing trial with early dysglycemia in 8-10 weeks of gestation resulted in better maternal-fetal outcomes and reduced GDM conversion during pregnancy. This publication is important as the final results of our trial will be published soon.
Prevalence
India is one of the countries with diabetes in the world and has one of the highest rates of GDM in women, affecting more than 5 million women in the country each year [1].
India currently has the second highest number of people with type 2 diabetes in the world at 77 million; Almost half of these patients are women. IDF 2019 estimates that 6 million newborns in India alone are affected by some form of hyperglycemia (HIP) during pregnancy, 90% of which are due to GDM [1]. Therefore, all women should be tested for gestational diabetes, even if they are asymptomatic. Unfortunately, the diagnostic criteria are not the same. (Table-1)
Table – 1: Diagnostic Criteria used by International/National organizations for estimating gestational diabetes.
| Organization | Fasting Plasma Glucose mmol/dl or mg/dl | Glucose Challenge | 1 h Plasma Glucose mmol/dl or mg/dl | 2 h Plasma Glucose | 3 h Plasma Glucose |
| WHO1999 1 | ≥7.0 or 125 | 75gm OGTT | Not required | ≥7.8 or 140 mg/dl | Not required |
| WHO2 2013 | ≥5.1 or 92 | ≥10.0 or 180 | ≥8.5 or 153 mg/dl | ||
| ADA3/American college Obstetricians & Gynaecologist4 2018 | ≥ 5.3 or 95 | 100gm OGTT | ≥10.0 or 180 | ≥8.6 or 155 mg/dl | ≥7.8 or 140 mg/dl |
| ADIPS 5 2014 | ≥5.1 or 92 | ≥10.0 or 180 | ≥8.5 or 153 mg/dl | ||
| EASD6, 1991 | ≥7.0 or 125 | ≥10.0 or 180 | |||
| FIGO7, 2015 | ≥5.1 or 92 | ≥10.0 or 180 | ≥8.5 or 153 mg/dl | ||
| Diabetes Canada Clinical Practice Guidelines8, 2018 | ≥5.3 or 95 | 75gm OGTT | ≥10.6 | ≥8.9 or 160 mg/dl | Not required |
| IADPSG9 | ≥5.1 0r 92 | 75gm OGTT | ≥10.0 0r 180 | ≥8.5 or 153 mg/dl | Not required |
| DIPSI10 2014 | – | 75 gm OGTT, non-fasting | – | ≥7.8 or 140 mg/dl | Not required |
| NICE11 | ≥5.6 or 100 | ≥7.8 or 140 mg/dl | Not required |
Diabetes in Pregnancy: Global, Regional, and Indian Scenario
The global diabetes epidemic is on the rise. According to IDF Head Professor Andrew Boulton, diabetes has become an epidemic.
The global prevalence of diabetes is estimated to rise from 537 million in 2021 to 783 million in 2045, an increase of 46%. [1] Diabetes is common worldwide, and this is a concern; by 2021, there will be 74.1 million diabetics in India.
This increase may be due to the aging of the Population, physical inactivity, urbanization, and obesity. These conditions increase the risk of diabetes mellitus, but early life is a risk factor. As suggested in David Baker’s “Fetal origins of adult disease” hypothesis, pregnancy planning can significantly impact adult health and disease. Pregnancy can be defined as the process in which stress or stimulus during a sensitive or important period of fetal development permanently changes the structure, body, and metabolism and thus creates a predisposition to a disease in the elderly. Lifestyle changes and medical interventions have been reported to slow or delay the development of Type-2 diabetes mellitus in people affected by impaired glucose tolerance (IGT), the first line of defense. Maintaining normoglycemia in GDM or other vulnerable individuals is the best option to prevent developing type 2 diabetes (T2DM). Diabetes can be reversed or stopped through primary prevention. For primary prevention of diabetes mellitus, women with gestational diabetes (GDM) are considered an ideal group because their children are more likely to have diabetes, and most of them acquired T2DM. Gestational diabetes may be an important factor in diabetes and obesity.
By 2021, the Global prevalence of hyperglycemia in pregnancy (HIP) will be 21.1 million people, accounting for 16.7% of births to women aged 20-49. These individuals may experience some form of hyperglycemia during pregnancy; 80.3% of these were due to GDM [2].
Therefore, all women must be tested for GDM, even if they have no symptoms.
Figure 1 IDF atlas, 2021
Keywords: Gestational Diabetes Mellitus; Epidemiological Studies; South Asia, Prevalence, Hyperglycaemia in pregnancy, HIP, GDM, FOGSI Federation of Obstetrics and Gynaecology of India.
1. Introduction
Although gestational diabetes mellitus (DIP) can cause hyperglycemia (HIP) during pregnancy, gestational diabetes mellitus (GDM) is still first detected during pregnancy [1]. HIP, whether diagnosed before, is dangerous and causes severe hyperglycemia during pregnancy that persists after delivery. Gestational diabetes usually causes mild to moderate hyperglycemia that also develops
in 50-60 % of women within 5 years of delivery. Because pregnancy occurs naturally, it can cause insulin resistance. The resulting hyperglycemia in healthy women is compensated by pancreatic β-cell hyperplasia to meet the additional metabolism needs.
However, due to various genetic and environmental factors, GDM cannot be compensated, leading to hyperglycemia [2]. Although GDM is associated with maternal-fetal complications, there are additional concerns. After giving birth, women with GDM are 10 times more likely to develop T2DM type 2 diabetes than women without GDM. Strict screening, monitoring, and preventive measures for women with postpartum GDM can help reduce T2DM in individual patients and even in the Population as a whole. Due to the rise in the current global prevalence of T2DM, the postpartum period of women with GDM is important in all countries, particularly those with a history of Gestational diabetes mellitus (GDM).
India is the largest country by Population and has the second-highest number of adults with T2DM globally. This number is expected to increase over 75% in the next 25 years [2].
2. Gestational Diabetes in South East Asia
Although T2DM has become a global epidemic [8], seven countries in Southeast Asia (India, Afghanistan, Bhutan, Maldives, Nepal, Pakistan, Sri Lanka, and Bangladesh) are the most severely affected by Diabetes and GDM. Disease severity accounts for approximately one-third of the global burden of diabetes and prediabetes [3]. In 2019, there were 88 million adults with diabetes in Southeast Asia, of whom more than half (57%) were undiagnosed [3]. If the current trend continues, 114 million Indians will be affected by 2045[2], and India may surpass China as the D.M. capital of the world.
Estimates were available per IDF Atlas 2021 for seven IDF Southeast Asia (SEA) countries. All countries have relevant data except Bhutan for diabetes estimates in adults 20-79. Nine documents from six countries were used. Estimates for Bangladesh and Nepal are based on research over the past five years. The IDF estimates that the number of people with diabetes in Southeast Asia will increase by 68% to reach 152 million by 2045 [2].
Figure 2 Number and proportions of adults with undiagnosed diabetes Aged 20-79 years, per region, 2021
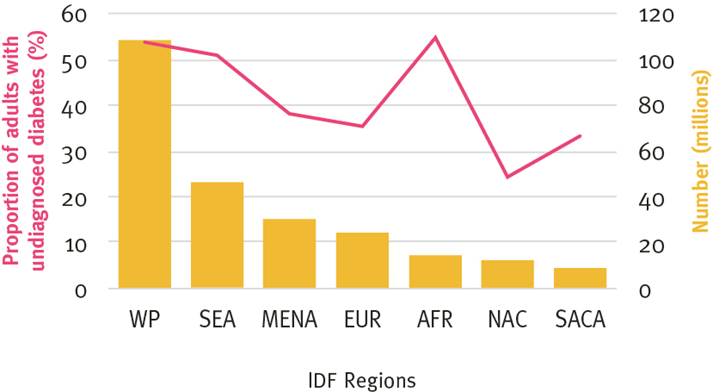
Figure 3 Hyperglycemia in pregnancy Per IDF region,2021
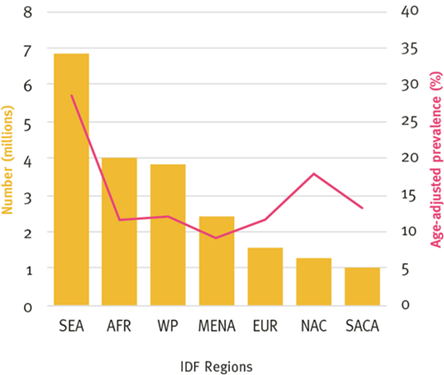
Therefore, the prevalence of GDM in Asia is higher than in Europe because Asians have more T2DM. Recent epidemiological data suggest that T2DM affects young women developing HIP during pregnancy. If immediate action and measures are not taken, morbidity and mortality from D.M. and GDM will continue unabated. However, as women make up half the Population and GDM is a major cause of T2DM, managing GDM early in pregnancy and postpartum screening help prevent T2DM from rising.
3. India: An example of global GDM trends
Globally, approaches to GDM are diverse and confusing, with little consensus. In the United States, the 1979 National Diabetes Dataset Guidelines was one of the earliest efforts to conduct an objective, systematic study of D.M. and GDM. After this initial Guideline and four international workshops on GDM (1979-1997), the recommendations proposed significant changes in the screening and diagnosis of GDM. Over the next two years, (ACOG & ADA) the American College of Obstetricians and Gynecologists and the American Diabetes Association (ACOG) followed this trend with new guidelines for GDM and HIP, Similar to the World Health Organization (WHO) 1980, 1985, 1999, and 2013. The Classification has also changed over time; Britain’s NICE National Institute for Health and Care Excellence, the Canadian Diabetes Association (CDA), and the Australian Gestational Diabetes Association (ADIPS) are some of the main standard-setting bodies (others) that use local and international research for updates. Therefore, over the past decade, due to international efforts, extensive research, and international consensus meetings, GDM treatment has seen an increase in screening, diagnosis, management, and postnatal care [5].
Thus, for example, separating GDM from DIP under the umbrella of HIP has clarified the meaning, and its relationship to HIP is now more clearly defined. In addition, the development and validation of diagnostic methods are very important as one universal Guideline. Countrywide is the need of time.
4. GDM prevalence in India
The prevalence of GDM in any given population depends on several factors, including characteristics of the study group: parental age, family history of diabetes, maternal weight and BMI, race, and ethnicity. Analysis of 84 studies showed that the combined prevalence of GDM in Asia was 11.5% (95% CI 10.9-12.0) [6]. However, there are significant differences in the majority of GDM due to differences in diagnostic criteria, screening methods, and work environments (e.g., urban and rural, home medical and community). Another study using data from 51 population studies found that the prevalence of GDM is affected by different diagnostic criteria.
In a study in the Indian Population using eight specialist diagnostic criteria for the same blood glucose results to diagnose OGTT, the prevalence of GDM ranged from 9.2% to 45.3%, depending on Therefore, most GDM in India ranges from 3.8% in Kashmir to 35% in Punjab [7].
Another review of 90 estimates from 64 studies showed that the prevalence of GDM in India ranged from 0% to 41.9%; the authors attribute this difference to different diagnosis models.
This study revealed large variations in the prevalence of GDM between regions. More importantly, the same standards were used (even in disease). The authors point out an important point: a different (other than “one size fits all”) approach will be costly in various parts of India.
5. Number of births with GDM in India
In India, 5-8 million women suffer from GDM each year [2]. India’s annual birth rate is about 25 million; this means that one-third of all babies will be affected by GDM. This information is based on the 2021 International Diabetes Federation (IDF) Atlas (10th edition), which states that 1 in 4 children born with HIP in Southeast Asia and 1 in 1 child worldwide has HIP [2]. In short, GDM is a bigger problem in India as it is more common.
Despite these challenges, it has encouraged Bangladesh, India, Pakistan, and Sri Lanka, the four largest countries responsible for more than 80 percent of the HIP burden live in Asia. With the help of policy experts, these schemes, federal and state grants, international organizations, and public health experts should conduct DIPSI tests on all pregnant women as blood sugar testing by hand using a glucometer is good today. Using a glucometer is common in Uttar Pradesh, Madya Pradesh, and other states under the National Health Mission funded program by Govt of India.
India faces a challenge for all countries with limited resources: how to apply the latest research within the constraints of personnel, laboratory equipment, and bureaucratic issues. There are also large cultural differences that create logistical problems. DIPSI screenings have the largest following in India and have been approved by the Govt of India MOHFW Guidelines 2014.
Because of differences in the prevalence of GDM in different states in India and given the country’s size, Experts agree that one method may not be suitable for all situations and that it is better to adapt to local solutions [1], a view shared by FIGO. The DIPSI test is still popular and accepted by major local organizations. So far, this is good practice.
With the high prevalence of Type 2 diabetes, there has been an increase in the incidence of GDM in India over the past two decades, mainly due to rapid changes in lifestyle, socioeconomics, and epigenetics that increase the prevalence of the disease. Indian women are estimated to have an 11 times higher risk of establishing GDM compared to women of other races and ethnicities. A 4 to 4 prevalence of GDM has been reported in India, 6% to 14% in urban parts of India and 1.7% to 13.2% in rural India. Overall, the incidence is between 3.8% and 17%. The majority in different parts of India is 9%, ranging from 35% in states like Punjab [2] to 17.9% in southern states like Tamil Nadu. [3] A lower rate of GDM (3.8%) has been reported in some regions, such as Kashmir. [4] A community study by Seshiah V et al. in South India showed that GDM prevalence in urban areas was 17%.8% compared to 9.9% in rural areas and 13.7%, similar to the population-based study with NHM in Uttar Pradesh [5]. Some diagnoses to arrive at GDM diagnosis for future diabetes prevention in India suggested. The Gestational Diabetes Working Group of India (DIPSI) [6] supports “one step” for the diagnosis of GDM, which is recommended by the NHM guidelines, GOI [7] for GDM (with or without fasting OGTT).
There are many reviews for all pregnant women. The onset of GDM in pregnant women can be delayed and is called true GDM. Many studies have been published to explain overt or true GDM formation. The severity of true GDM represents only the tip of the GDM disease iceberg. However, there are many cases of latent gestational diabetes (PGDM) in the Population resulting from Type-1DM or Type 2 diabetes before pregnancy. Although the prevalence of PGDM in India is low, due to the long duration of hyperglycemia and its impact on children’s health, these women are at high risk for many complications, such as macrosomia, neonatal diabetes, and polyhydramnios. A study by Fang W et al. shows that the prevalence of PGDM is 0.66%. This proportion of Asians [8] is lower than for other races. However, these women often suffer from many diseases, such as thyroid disease, high blood pressure, and pyelonephritis, that cause fertility problems.
Risk Factors: Many risk factors have been identified for GDM, including race, ethnicity, age, BMI body mass index, type 2 diabetes in first-generation relatives, history of GDM, macrosomia, and death in a previous pregnancy. History of recurrent miscarriage, weight gain, polycystic ovary syndrome (PCOS), polyhydramnios, and metabolic syndrome [9]
6. Obesity
According to an unhealthy lifestyle, risk factors for GDM can be divided into variable and non-variable. Things change. Modifiable risk factors include many lifestyle risks, including physical inactivity, poor diet, obesity, smoking, alcohol consumption, and other environmental risk factors. The main metabolic risk factors include obesity and poor diet. Obesity is another metabolic disease that increases body mass index (BMI). Retrospective studies have shown that more than 70% of women with GDM are overweight or obese, thus at risk for the disease. A meta-analysis by Chu et al. showed that the risk of GDM increases significantly as pre-pregnancy BMI increases, 2.14-fold for obese women and 3.56-fold for obese women [10], leads to additional complications during pregnancy, causing many antenatal and perinatal complications, and can also increase the risk of postpartum diabetes. The underlying pathophysiology linking obesity to GDM is insulin resistance.
Obesity is a chronic, low-grade disease that begins in adipose tissue and progresses to major organs, including the liver and pancreas, and chronic inflammation in adipose tissue causes insulin resistance by blocking insulin receptors and inhibiting insulin signaling. The effects of obesity and GDM on infants have been extensively studied, and both maternal obesity and GDM have been identified as risk factors for obese children. Babu GR et al. They found that GDM mediated 25% of the total effect of maternal obesity and obesity, with a difference of 2.2 for overall significance [11].
7. Physical inactivity
Another important risk modifier for GDM is physical inactivity. Limiting physical activity and exercise during pregnancy is a common practice to prevent uterine contractions. However, studies show that only 10 percent of pregnant women participate in recommended physical activity levels. Anjana RM et al. also found that women with GDM tended to be restricted in activities compared to women without GDM, which increased the risk of GDM [12]. Therefore, a sedentary lifestyle is a risk factor for obesity and GDM. As the tendency to be sedentary increases during pregnancy, especially in the third trimester, energy consumption decreases, making a negative impact on glucose and thus increasing the incidence of GDM. Several clinical studies comparing the effect of exercise on the glycaemic index have shown that at least six weeks of ergometric exercise or low-intensity work in pregnant women can reduce fasting and postprandial blood glucose outcomes. Mishra S et al. Another study on GDM found that women with GDM did low to moderate physical activity [13] and also noted that when pregnant women were physically active, they had a higher risk of GDM compared to participants of 3000 METs and above. Physical exercise minutes per week, <2999 MET minutes per week (p < 0.001). Although physical inactivity is said to be a risk factor for GDM, some studies have failed to provide a connection between physical activity and diabetes. Additionally, the need for appropriate guidelines with specific recommendations for the field of physical activity in this population is problematic when making recommendations for physical therapy.
8. Diet
According to the Finnish Gestational Diabetes Prevention Study (RADIEL study), the GDM risk was 40% lower with moderate physical activity and a healthy diet [14], which brings us to the most important part of the healthy living way. GDM is a metabolic disease mainly associated with carbohydrate metabolism and influenced by diet. A healthy diet includes adequate food preparation, appropriate portions, and healthy foods. For GDM, it is important to prepare foods that are low in glycaemic index and high in Fibre to support the proper functioning of the pancreas and insulin secretion.
In a study by Chen et al., greater consumption of soft drinks and sugar increases the risk of GDM, including various hot and cold beverages, most of which contain caffeine, cola, beer, and spirits [15]. According to a 2008 Cochrane review, eating a low-glycemic diet and avoiding refined and processed foods during pre-pregnancy can reduce the risk of GDM during pregnancy. According to a study by Sedagat F et al., consumption of healthy Western foods (such as jam, mayonnaise, salty foods, and foods such as processed meats and eggs) is associated with an increased risk of GDM compared to nonsmokers. Western dietary patterns have an odds ratio of 1.97 for this substance [16]. A diet rich in a Mediterranean diet and vegetables were correlated with a lower risk of GDM [17,18]. In comparison, red meat and processed refined carbohydrates were associated with a significantly higher risk of GDM. The early education, dietary advice, and therapy before 20 weeks of gestational in GDM results in better composite neonatal outcomes in the TOBOGM trial results [19].
9. Smoking
Smoking and not smoking are risk factors for many diseases, such as cancer. These toxins have potential carcinogenic, atherogenic, and teratogenic effects. We take strict measures to prevent addiction to tobacco products. In experimental animal studies, smoking has been positively associated with hyperinsulinemia and insulin resistance. Despite the lower prevalence of smoking products in India, it is important to assess the risk of GDM associated with it. According to a study by Terry PD et al., there was no significant association between smoking and GDM in first-time mothers [20].
In another study by Bar-Zeev Y et al., it was shown that there is a risk of GDM with an odds ratio of 1.25 in mothers who smoked during pregnancy, and this risk increases with smoking[21].
It is important to reduce modifiable risks through primary prevention, as primary prevention is sufficient to prevent GDM. Early health education is needed to prevent complications due to GDM, promoting the importance of a healthy lifestyle, diet, and exercise. However, many irreversible risks pose serious problems for doctors for whom secondary prevention strategies such as early detection and treatment will help.
Some of these non-modifiable risk factors are advanced age, multiple pregnancies, infertility, multiple pregnancies, and a family history of GDM.
10. Advanced Primiparous and Advanced Maternal Age
Maternal age is an important indicator of many pregnancy complications, including miscarriage, fetal growth retardation, gestational hypertension, and GDM. Also, increasing maternal age during pregnancy can lead to many complications, including diabetes and high blood pressure, and can lead to further complications. A meta-analysis by Li Y et al. found that, compared with women in the 20-24 age group, women under 20 have a lower risk of GDM, which increases steadily with age, while women over 40 have a lower risk of GDM. A 3.78-fold increase in age is associated with a 3.78-fold increased risk of developing GDM [22].
When comparing the risk between 30-34 years and 20-24 years of age by ethnicity, Asians showed a higher risk of GDM with a potential difference of 1.79 compared to European countries with an odds ratio of 5.77 [22]. A study by Mahalakshmi MM et al. in India evaluated a group of 29-year-old South Indian pregnant women, 6.3% of whom had GDM [23].
11. Twin Pregnancy
Another important factor that does not change the risk of developing GDM is a twin pregnancy. According to a study by Rauh-Hain JA et al., the presence of twins increases the risk of GDM compared to singleton pregnancies (3.98% and 2.32%, respectively) and is significant.
In addition, women who have twin pregnancies between the ages of 25-30 are more likely to have this condition. As a result, the hospitalization of pregnant boys in the HDU high HDU-dependent unit or neonatal intensive care unit (NICU) has increased [24]. These children may also suffer from respiratory problems. Although potential risks have been explored, the relationship between these two risks is unclear. In a retrospective study by Sheehan ACM et al., twin pregnancies were associated with pregnancy-related complications and neonatal hypoglycemia in infants, thus increasing the risk of GDM [25]. However, macrosomia was not observed in this study.
More evidence from the Indian Population is needed to establish a causal link between twin pregnancy and GDM.
12. Infertility and PCOS
Polycystic ovary syndrome (PCOS) is a hormonal disorder characterized by insulin resistance and irregular menstruation in women of reproductive age. These women are at high risk of GDM because of the hyperinsulinemia state and insulin resistance combined with high plasma androgen levels. A study examining the impact of PCOS on pregnancy by Foroozanfard F et al. showed that women with PCOS and GDM were more than three times as likely to develop preeclampsia and PIH; Maternal PCOS and GDM are also associated with an increase in neonatal diabetes. These findings highlight the risk link between PCOS and GDM. [26]
Infertility poses an important direct and indirect risk for GDM. It has been determined that pregnant women who use birth control methods have a higher risk than women who are pregnant during pregnancy. Although the exact mechanism is unknown, research has shown that older women may be the cause of glucose intolerance in women, thus predisposing them to the risk of GDM.
13. Family history of GDM and risk of future diabetes
Although many risk factors are considered, one of the most important and unchanging risk factors is a family history of GDM. Many studies have investigated the role of genetic markers in GDM risk.
In Iran, Moosazadeh M et al. In a study by A.D., individuals with a positive family history had a 3.46-fold higher risk of developing GDM compared with those without a family history [27]. In India’s largest study in Uttar Pradesh, Jain et al. reported 2.62 times the relative risk for GDM in a large UP population study. About 50 out of 100 pregnant women with a history of GDM develop type 2 diabetes within five to ten years after birth [28]
14. Uric Acid, Creatinine and albumin and GDM: A new Risk factors
The findings of various studies confirm the association of uric acid with GDM. Importantly, the early pregnancy uric acid levels in the present study were similar to those reported by others, suggesting that these findings may apply to a broader population of pregnant women.
Sahin Aker S et al. found that GDM can be predicted with 100% sensitivity using a serum uric acid cut-off of 3.95 mg/dL [29]. Also, Zhou J et al. measured lipids and uric acid in 1000 women at 20 weeks of gestation and found that increased uric acid is associated with a two-fold risk for preeclampsia and a 2.34-fold risk for GDM [30].
New findings from India show that first-trimester uric acid levels>3.35 mg/dL exhibit a sensitivity of 100% and specificity of 84.2% for predicting GDM. The predictive modeling employed demonstrated the superior accuracy of the model containing uric acid, creatinine, and albumin, which had a higher correlation (r=0.82) with Plasma Glucose (PG) compared to other models [31]. This high level of accuracy should provide confidence in the reliability of our findings. It is possible to predict the advance of GDM early in the first trimester using this predictive model of biochemical values with high accuracy.
In India, Ist trimester screening advocated by Seshiah et al., during 8-10 Weeks of Gestation, and the use of Metformin in early dysglycemia ≥110 mg/dl resulted in Gestational Diabetes prevention and better Maternal-fetal outcomes; the trial is still ongoing, and the results will be soon published [32].
Summary:
India has made tremendous progress worldwide in achieving HIP pregnancy Screening through the “Universal Single Test Procedure” advocated by DIPSI and adopted by the Government of India, MOHFW 2014 Guidelines.
The importance of GDM management is simple: If diagnosed, treated, and followed up after birth, it will reduce the burden of T2DM in a country now and in future generations. Therefore, GDM monitoring has the potential to change future predictions regarding T2DM.
Specifically, 90% of HIP births occur in low- and middle-income countries. There are significant challenges in universal screening for GDM, with coverage rates ranging from 10% to 90%. Missing out or not treating women with GDM leads to short-term and long-term complications associated with GDM.
Overall, it is important to consider GDM preventable, provided adequate risks are considered in the pre-conception stage. There is a need to educate the population at large on the dangers and impact of GDM on the mother and the fetus to initiate early preventive strategies, such as adopting a healthy lifestyle, pre-conception counseling, identifying risk factors, and screening every pregnant woman for GDM as soon as possible.
Early GDM Screening and Management is key for GDM Prevention and better Maternal foetal outcomes and for curtailing the epidemic of Type 2 diabetes around the Globe.
References:
- International Diabetes Federation.IDF Diabetes Atlas, 10th ed. Brussels, Belgium: International Diabetes Federation, 2021. Available at: https://www.diabetesatlas.org
2. Mantri, N., Goel, A.D., Patel, M. et al. National and regional prevalence of gestational diabetes mellitus in India: a systematic review and Meta-analysis. BMC Public Health 24, 527 (2024). https://doi.org/10.1186/s12889-024-18024-9
3. Seshiah V, Balaji V, Balaji MS, Sanjeevi CB, Green A. Gestational diabetes mellitus in India. J Assoc Physicians India. 2004; 52: 707-11.
4. Raja MW, Baba TA, Hanga AJ, Bilquees S, Rasheed S, Haq IU et al. A study to estimate the prevalence of gestational diabetes mellites in an urban block of Kashmir valley (North India). Int J Med Sci Public Health. 2014; 3(2): 191-195
5. Jain R, Davey S, Arya S, Davey A, Raghav SK. A prospective study with outcome on gestational diabetes mellitus. J Evol Med Dent Sci. 2015; 4: 15640‑7.
6. Seshiah V, Das AK, Balaji V, Joshi SR, Parikh MN, Gupta S; Diabetes in Pregnancy Study Group. Gestational diabetes mellitus–guidelines. J Assoc Physicians India. 2006; 54: 622-8.
7. Ministry of health & family Welfare GOI. Diagnosis & Management of Gestational Diabetes Mellitus Technical and Operational Guidelines. [Internet]. 2018 Available from https://nhm.gov.in/New_Updates_2018/NHM_Components/RMNCH_MH_Guidelines/Gestational-Diabetes-Mellitus.pdf
8. Fong A, SerraA, Herrero T, Pan D, Dotun Ogunyemi.Pre-gestational versus gestational diabetes: a population-based study on clinical and demographic differences. J Diabetes complications. 2014; 28(1): 29-34.
9. Berger H, Crane J, Farine D et al. Screening for gestational diabetes mellitus. J Obstet Gynaecol Can. 2002; 24: 894e912
10. Chu SY, Callaghan WM, Kim SY, et al. Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care 2007;30(8):2070–2076
11. Babu GR, Deepa R, Lewis MG, Lobo E, et al. Do Gestational Obesity and Gestational Diabetes Have an Independent Effect on Neonatal Adiposity? Results of Mediation Analysis from a Cohort Study in South India. Clin Epidemiol. 2019 Dec 27; 11:1067-1080.
12. Anjana RM, Sudha V, Lakshmipriya N, Anitha C, et al. Physical activity patterns and gestational diabetes outcomes – The wings project. Diabetes Res Clin Pract. 2016 Jun; 116:253-62.
13. Mishra S, Kishore S. Physical activity during pregnancy affects gestational diabetes mellitus. Indian J Endocr Metab.2018; 22:661-71. Available from: http://www.ijem.in/text.asp?2018/22/5/661/241493
14. Koivusalo SB, Rönö K, Klemetti MM, et al. Gestational Diabetes Mellitus Can Be Prevented by Lifestyle Intervention: The Finnish Gestational Diabetes Prevention Study (RADIEL): A Randomized Controlled Trial. Diabetes Care. 2016 Jan;39(1):24-30.
15. Chen et al. Prospective Study of Pre-Gravid Sugar-Sweetened Beverage Consumption and the Risk of Gestational Diabetes Mellitus. Diabetes Care, 2009; 32 (12): 2236
16. Fatemeh Sedaghat, Mahdieh Akhoondan, Mehdi Ehtes et al. Maternal Dietary Patterns and Gestational Diabetes Risk: A Case-Control study. Journal of Diabetes Research.2017;5173926:1-8
17. Pham NM, Do VV, Lee AH. Polyphenol-rich foods and risk of gestational diabetes: a systematic review and meta-analysis. Eur J ClinNutr. 2019; 73(5): 647-656
18. Shin D, Lee K, Song W. Dietary patterns during pregnancy are associated with risk of gestational diabetes mellitus. Nutrients. 2015; 7: 9369–82.
19. Simmons D, Immanuel J, Hague WM, Teede H, Nolan CJ, Peek MJ, Flack JR, McLean M, Wong V, Hibbert E, Kautzky-Willer A, Harreiter J, Backman H, Gianatti E, Sweeting A, Mohan V, Endicott J, Cheung NW; TOBOGM Research Group. Treatment of Gestational Diabetes Mellitus Diagnosed Early in Pregnancy. N Engl J Med. 2023 Jun 8;388(23):2132-2144. doi: 10.1056/NEJMoa2214956
20. Terry PD, Weiderpass E, Östenson CG, Cnattingius S. Cigarette Smoking and the Risk of Gestational and Pregestational Diabetes in Two Consecutive Pregnancies. Diabetes Care. 2003; 26(11): 2994-2998.
21. Bar-Zeev, Yael PhD, MD; Haile, Zelalem T. PhD, MPH; Chertok, Ilana Azulay PhD, MSN. Association Between Prenatal Smoking and Gestational Diabetes Mellitus. Obstetrics & Gynecology. 2020; January 2020 (35): 1(91-99)
22. Yueyi Li a, Xinghua Ren b, Lilan He, et al. Maternal age and the risk of gestational diabetes mellitus: A systematic review and meta-analysis of over 120 million participants. Diabetes research and Clinical Practice.2020;162:108044
23. Mahalakshmi MM, Bhavadharini B, Kumar M, et al. Clinical profile, outcomes, and progression to type 2 diabetes among Indian women with gestational diabetes mellitus seen at a diabetes center in south India. Indian J Endocrinol Metab. 2014 May;18(3):400-6.
24. Rauh-Hain JA, Rana S, Tamez H, Wang A, et al. Risk for developing gestational diabetes in women with twin pregnancies. J Matern Fetal Neonatal Med. 2009; 22(4): 293-299
25. Annabel C. M. Sheehan, Mark P. Umstad, Stephen Cole, and Thomas J. Cade. Does gestational diabetes cause additional risk in twin pregnancy? Twin Research and Human Genetics.2019; 1–8
26. Foroozanfard f, Moosavi SGA, Mansouri F, et al. Obstetric and Neonatal Outcome in PCOS with Gestational Diabetes Mellitus, J Family Reprod Health. 2014 Mar; 8(1): 7–12.
27. Moosazadeh M, Asemi Z, Lankarani KB, et al. Family history of diabetes and the risk of gestational diabetes mellitus in Iran: A systematic review and meta-analysis. Diabetes Metab Syndr. 2017;11 (Suppl) 1:S99-S104.
28. Jain R, Davey S, A, Raghav SK, Singh JV. Can the management of blood sugar levels in gestational diabetes mellitus cases be an indicator of maternal and fetal outcomes? The results of a prospective cohort study from India. J Fam Community Med. 2016; 23:94-9.
29. Sahin Aker S, Yuce T, Kalafat E, Seval M, Söylemez F. Association of first-trimester serum uric acid levels gestational diabetes mellitus development. Turk J Obstet Gynecol. 2016;13(2):71-74
30. Zhou J, Zhao X, Wang Z, Hu Yali. A combination of lipids and uric acid in the mid-second trimester can be used to predict adverse pregnancy outcomes. J Matern Fetal Neonatal Med. 2012; 25:2633-38.
31. Palaniappan Y, Samal S, Lakshmi M, Prabhu K. First Trimester Prediction of Gestational Diabetes using a Predictive Model of Biochemical Parameters-A Longitudinal Study. Journal of Clinical & Diagnostic Research. 2022 Sep 1;16(9). DOI: 10.7860/JCDR/2022/55641.16831
32. Seshiah V, Bronson SC, Balaji V, Jain R, Anjalakshi C. Prediction and Prevention of Gestational Diabetes Mellitus and Its Sequelae by Administering Metformin in the Early Weeks of Pregnancy. Cureus. 2022 Nov 15;14(11): e31532. Doi: 10.7759/cureus.31532
- Acknowledgment: We would like to express our deepest gratitude to Dr V Seshiah for their invaluable guidance and support throughout the research process.
- Funding
Not applicable
- Informed Consent
Not applicable
- Conflict of Interest Statement
All the authors declared “No Conflict of Interest” with this publication.
- Additional Information
Not applicable
This open-access article is distributed under the terms of the Creative Commons Attribution License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
- DOI: 10.62996/daj.09072024
Cite this article: Rajesh Jain1*, Veeraswamy Seshiah2 N, Guneeta Mehta Jain3, Pikee Saxena4, 5Shaily Agarwal, 6Sadhana Tiwari. Epidemiology of Gestational Diabetes Mellitus: Newer Evidence to curtail. Diabetes Asia Journal. 2024; 1(1):60-55. https://doi.org/10.62996/daj.09072024

