Veeraswamy Seshiah1, Anjalakshi C2, Bhavatharini N3, Geetha Lakshmi A4, Shanmugam A5, Pikee Saxena6, Dr Rajesh Jain7
1Distinguished Professor, The Tamil Nadu Dr. M.G.R. Medical University, Chennai, Tamil Nadu; 2Department of Obstetrics Gynaecology, Madha Medical College and Research Institute, Chennai; 3SRC Diabetes Centre, Erode, Tamilnadu; 4Department of Obstetrics and Gynaecology, RSRM hospital, Stanley Medical College, Chennai; 5Dr Ambedkar Institute of Diabetes, Govt Kilpauk Medical College & Hospital, Chennai-10; 6 Department of Obstetrics and Gynaecology, Lady hardinge Medical college, New Delhi, 7Jain Hospital & Research Centre, Kanpur, India
Submitted: 14 May 2024; Accepted: 05 June Dec 2024; Published: 27 June 2024
Correspondence Author: Dr V Seshiah, Email: [email protected]
Key Words: Early Gestational Glucose Intolerance (EGGI), Early Gestational Diabetes Mellitus (eGDM), Diabetes in Pregnancy Study Group India (DIPSI), Metformin, Medical Nutrition Therapy (MNT). National institute of health (NIH).
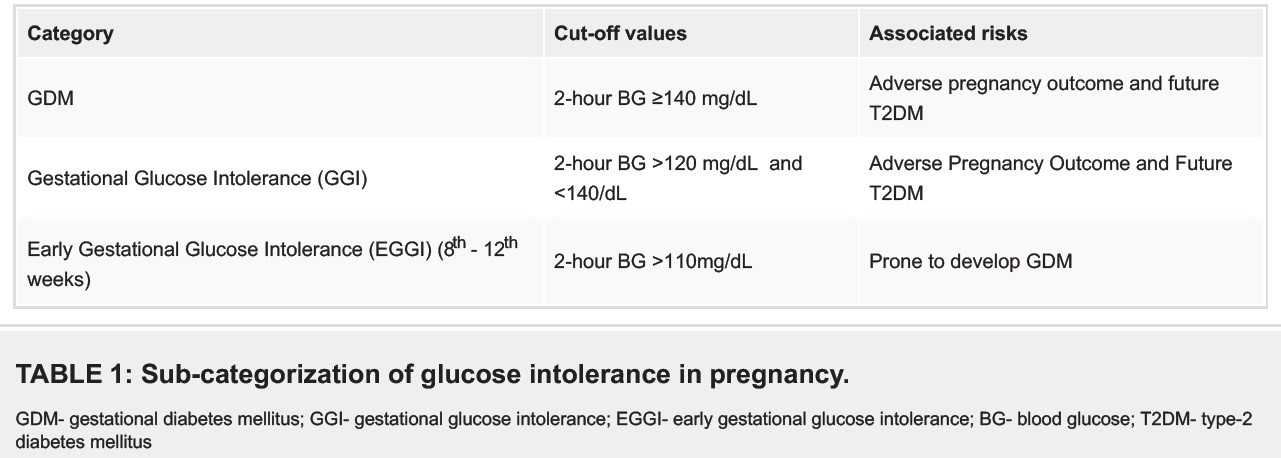
The NIH recommends screening at the 10th week of pregnancy because the fetal beta cell begins insulin secretion at the 11th week of gestation. Abnormal prandial glycaemic levels may stimulate beta cell secretion. According to the pattern of glycemia in normal pregnancy, if the postprandial blood sugar (PPBS) in the 10th week is greater than 110 mg/dl, it predicts gestational diabetes mellitus (GDM)[1]. Therefore, it is important to bring blood glucose levels to less than 110 mg/dl, as fetal beta cells start secreting insulin around 10-11 weeks, which leads to changes in maternal metabolism[2]. Given this background, there is a need to lower the cut-off to detect glucose intolerance, especially in the early weeks of pregnancy. With this in mind, a practical sub-categorization of glucose intolerance in pregnancy has been proposed (Table 1)[3]. The DIPSI Diabetes in Pregnancy Study Group in India, a pioneer in developing the DIPSI Test, has suggested conducting universal screening earlier in pregnancy, around the 8th to 10th weeks, to predict the risk of gestational diabetes (GD). This early prediction allows for the introduction of metformin and specialized medical nutritional treatment for women with glycemic abnormalities in the latter part of the first trimester[3].
Credit: V Seshiah
Why are Indians more prone to Type 2 Diabetes mellitus (T2DM)?
The typical South Asian Phenotype has the following features, which makes them more prone to Type 2 Diabetes mellitus.
- Low birth weight – “Thin, fast Indian.” (FTO)[4]
- Lower age of onset.
- Lower threshold for BMI.
- Increased serum insulin levels and insulin resistance.
- Rapid decline in beta cell function.
- Characteristic dyslipidemia – low HDL cholesterol, elevated Triglycerides, and small dense LDL.
- Low levels of adiponectin.
- Increased level of inflammatory markers – High sensitivity – C-reactive protein (Hs-CRP), IL-6
- Low muscle mass.
- Increased abdominal obesity and visceral fat
- Increase Steatotic liver disease (SLD) (old terminology – non-alcoholic fatty liver disease- NAFLD).
Guidelines currently recommend standard screening for gestational diabetes mellitus (GDM) at 24–28 weeks of pregnancy, with early screening offered to those deemed high-risk. The International Federation of Gynaecology and Obstetrics (FIGO) strongly recommends that all pregnant women undergo early screening for hyperglycemia during pregnancy using a Single Test procedure[5]. The Diabetes in Pregnancy Study Group of India (DIPSI) recommends universal screening for all pregnant women during the first trimester using a simple, cost-effective, and feasible Single Test procedure involving a 75-gm glucose challenge to diagnose GDM[6]. DIPSI’s guideline captures pregnant women with high insulin resistance as reflected in the Postprandial Blood Glucose ≥140 mg/dl. The IADPSG Guidelines recommend that GDM be diagnosed if any one value is abnormal in OGTT, but the diagnosis can only be made if OR=1.5 is implemented rather than 1.75 [7].
A study from Italy that used both DIPSI and IADPSG criteria in the same pregnant women found that both guidelines had almost the same prevalence but missed cases of GDM due to different criteria [8]. In a multi-centric study including India with a high incidence of hyperglycemia during pregnancy, the Towards a Better Outcomes in Gestational Diabetes Mellitus (TOBOGM) study emphasizes the critical importance of early screening at the beginning of pregnancy, followed by tailored interventions for identified GDM cases. The study found a 24.9% adverse neonatal outcome rate in the immediate treatment group and a 30.5% rate in the control group, although after adjustment, the risk difference was non-significant[9]. In Nigeria, Africa, a cross-sectional comparison of universal and selective risk factor-based screening for GDM found that selective risk factor-based screening missed 31.11% of patients with GDM compared to universal screening using a 75g oral glucose tolerance test OGTT[10]. There’s an interest in investigating if a similar scenario exists for GDM when screening is limited to high-risk patients[11].
Picture 1: Primordial Prevention of Diabetes
There is a pressing need to differentiate Early Gestational Glucose Intolerance (EGGI) from eGDM diagnosis (<24 weeks or average gestational age of 15.6 ± 2.5 weeks in the TOBOGM study). In contrast, the usual practice is to diagnose after 24 weeks. This differentiation is crucial and should be a priority in maternal and fetal health care.
In summary, the evidence and experiences we have presented strongly advocate for the implementation of universal Early Gestational Glucose Intolerance (EGGI) By 10thWeek of gestation with ≥110 mg/dl value, timely identification and intervention with MNT & Metformin can significantly improve pregnancy outcomes.
References
1. Hinkle SN, Tsai MY, Rawal S, Albert PS, Zhang C. HbA1c measured in the first trimester of pregnancy and the association with gestational diabetes. Sci Rep. 2018; 8:12249. https://doi.org/10.1038/s41598-018-30833-8.
2. Hernandez TL, Friedman JE, Van Pelt RE, Barbour LA. Patterns of glycemia in normal pregnancy: should the current therapeutic targets be challenged? Diabetes Care. 2011 Jul;34(7):1660–8
3. Seshiah V, Bronson SC, Balaji V, Jain R, Anjalakshi C. Prediction and prevention of gestational diabetes mellitus and its sequelae by administering metformin in the early weeks of pregnancy. Cureus. 2022; 14(11):e31532.
4. Kapoor N. Thin Fat Obesity: The Tropical Phenotype of Obesity. [Updated 2021 Mar 14]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568563/
5.Hod M, Kapur A, Sacks DA, et al. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: a pragmatic guide for diagnosis, management, and care. Int J Gynaecol Obstet 2015;131 Suppl 3: S173–S211.
6. Seshiah V, Balaji V, Bronson SC, Jain R, Chandrasekar A. Diagnosing Gestational Diabetes by a Single-Test Procedure Is a Propitious Step Towards Containing the Epidemic of Diabetes. Cureus. 2021 Nov 25;13(11):e19910. doi: 10.7759/cureus.19910
7. Seshiah V, Shah SS, Balaji V, Anjalakshi C, Jain R. When are we Going to Settle the Diagnostic Criteria of Gestational Diabetes Mellitus? J Assoc Physicians India. 2019 Oct;67(10):70-72. https://pubmed.ncbi.nlm.nih.gov/31571457/
8. Patients (Corrado F, Di Benedetto A, Di Vieste G, La Fauci L, Martinelli C, D’Anna R, Pintaudi B. Diagnosing Gestational Diabetes with a Probably Too Simplified Diagnostic Procedure Compared to International Criteria: The Indian Case Study. J Clin Med. 2022 Jun 28;11(13):3745. doi: 10.3390/jcm11133745)
9. Simmons D, Immanuel J, Hague WM, Teede H, et al. TOBOGM Research Group. Treatment of Gestational Diabetes Mellitus Diagnosed Early in Pregnancy. N Engl J Med. 2023 Jun 8;388(23):2132-2144. doi: 10.1056/NEJMoa2214956
10. Nwali SA, Onoh RC, Dimejesi IB, et al. Universal versus selective screening for gestational diabetes mellitus among antenatal clinic attendees in Abakaliki: using the one-step 75-gram oral glucose tolerance test. BMC Pregnancy Childbirth 2021; 21 (1): 735.
11. Sundarka MK, Sundarka A. Early Gestational Diabetes Mellitus: An Update. J Assoc Physicians India. 2024 Mar;72(3):108. doi: 10.59556/japi.72.0470
Early Gestational Glucose Intolerance (EGGI) Diagnosis and Prevention of Diabetes
Submitted: 14 May 2024; Accepted: 05 June Dec 2024; Published: 27 June 2024
Veeraswamy Seshiah1, Anjalakshi C2, Bhavatharini N3, Geetha lakshmi A4, Shanmugam A5, Pikee Saxena6, Dr Rajesh Jain7
Corresponding Author: Correspondence Author: Dr V Seshiah, 1Distinguished Professor, The Tamil Nadu Dr. M.G.R. Medical University, Chennai, Tamil Nadu Email: [email protected]
- Acknowledgment
Not applicable
- Funding
Not applicable
- Informed Consent
Not applicable
- Conflict of Interest Statement
All the authors declared “No Conflict of Interest” with this publication.
- Additional Information
Not applicable
This open-access article is distributed under the terms of the Creative Commons Attribution License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
- DOI: 62996/daj.02072024
- Cite this Article
Veeraswamy Seshiah1, Anjalakshi C2, Bhavatharini N3, Geetha lakshmi A4, Shanmugam A5, Pikee Saxena6, Dr Rajesh Jain7. Early Gestational Glucose Intolerance (EGGI) Diagnosis and Prevention of Diabetes. Diabetes Asia Journal. 2024;1(1):3-7. https://doi.org/10.62996/daj.02072024

