novel coronavirus-2019 Covid-19

Coronavirus disease (COVID-19) pandemic
novel coronavirus-2019 Covid-19
novel coronavirus-2019 Covid-19
novel coronavirus-2019 Covid-19
novel coronavirus-2019 Covid-19
Reporting
Infection fatality ratio (IFR)
Case fatality ratio (CFR)
Mitigation
Main article: Public fitness mitigation of COVID-19
Contact tracing
Health care
History
Main article: Timeline of the COVID-19 pandemic
Asia
China
India
novel-coronavirus-2019: Covid-19
The ongoing global pandemic of coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The virus was first identified on 17 November 2019 in Wuhan, China. The World Health Organization declared a Public Health Emergency of International Concern on 30 January 2020 and later declared a pandemic on 11 March 2020. As of 8 July 2021, more than 185 million cases have been confirmed, with more than 4 million confirmed deaths attributed to COVID-19, making it one of the deadliest pandemics in history.
The severity of COVID-19 symptoms is highly variable, ranging from unnoticeable to life-threatening. Severe illness is more likely in elderly COVID-19 patients and those who have certain underlying medical conditions. COVID-19 transmits when people breathe in air contaminated by droplets and small airborne particles. The risk of breathing these in is highest when people are nearby, but they can be inhaled over longer distances, particularly indoors. Transmission can also occur if splashed or sprayed with contaminated fluids in the eyes, nose, or mouth and, rarely, via contaminated surfaces. People remain contagious for up to 20 days and can spread the virus even if they do not develop any symptoms.
Recommended preventive measures include social distancing, wearing face masks in public, ventilation and air-filtering, hand washing, covering one’s mouth when sneezing or coughing, disinfecting surfaces, and monitoring and self-isolation for people exposed or symptomatic. Several vaccines have been developed and widely distributed in most developed countries since December 2020. Current treatments focus on addressing symptoms, but work is underway to develop medications that inhibit the virus. Authorities worldwide have responded by implementing travel restrictions, lockdowns and quarantines, workplace hazard controls, and business closures. Numerous jurisdictions have also worked to increase testing capacity and trace contacts of the infected.
The pandemic has resulted in severe global, social, and economic disruption, including the largest global recession since the Great Depression of the 1930s. It has led to widespread supply shortages exacerbated by panic buying, agricultural disruption, and food shortages. However, it has also caused temporary decreases in emissions of pollutants and greenhouse gases. Numerous educational institutions and public areas have been partially or fully closed, and many events have been canceled or postponed. Misinformation has circulated through social media and mass media, and political tensions have been exacerbated. The pandemic has raised racial and geographic discrimination, health equity, wealth inequality, and the balance between public health imperatives and individual rights.
Background
Although the exact origin of the virus is still unknown, the first outbreak started in Wuhan, Hubei, China, in late 2019. Many early cases of COVID-19 were linked to people who had visited the Huanan Seafood Wholesale Market in Wuhan. Still, it is possible that human-to-human transmission was already happening before this. On 11 February 2020, the World Health Organization (WHO) named the disease “COVID-19”, short for coronavirus disease 2019. The virus that caused the outbreak is known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a newly discovered virus closely related to bat coronaviruses, pangolin coronaviruses, and SARS-CoV. The current scientific consensus is that the virus is most likely of zoonotic origin, from bats or another closely related mammal. Despite this, the subject has generated a significant amount of speculation and conspiracy theories amplified by rapidly growing online echo chambers. Global geopolitical divisions, notably between the United States and China, have been heightened because of this issue.
The earliest known person with symptoms was later discovered to have fallen ill on 1 December 2019, and that person did not have visible connections with the later wet market cluster. However, an earlier case of infection could have occurred on 17 November. Of the early cluster of cases reported that month, two-thirds were linked with the market. Molecular clock analysis suggests that the index case is likely to have been infected with the virus between mid-October and mid-November 2019.
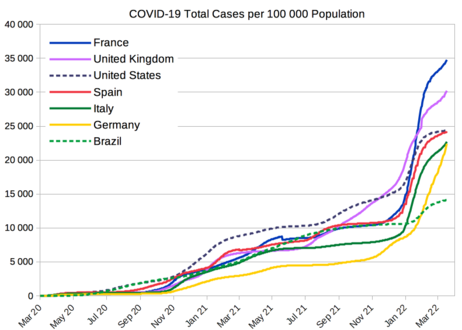
Cases
Official case counts refer to the number of people tested for COVID-19 and whose test has been confirmed positive according to official protocols. Many countries, early on, had official policies not to test those with only mild symptoms. An analysis of the early phase of the outbreak up to 23 January estimated 86 percent of COVID-19 infections had not been detected. These undocumented infections were the source of 79 percent of documented cases. Using various methods, several other studies have estimated that the numbers of infections in many countries are likely to be considerably greater than the reported cases.
On 9 April 2020, preliminary results found that 15 percent of people tested in Gangelt, the center of a major infection cluster in Germany, tested positive for antibodies. Screening for COVID-19 in pregnant women in New York City, and blood donors in the Netherlands, has also found rates of positive antibody tests that may indicate more infections than reported. Seroprevalence-based estimates are conservative as some studies show that persons with mild symptoms do not have detectable antibodies. Some results (such as the Gangelt study) have received substantial press coverage without first passing through peer review.
An analysis in early 2020 of cases by age in China indicated that a relatively low proportion of cases occurred in individuals under 20. It was not clear whether this was because young people were less likely to be infected or less likely to develop serious symptoms, seek medical attention, and be tested. A retrospective cohort study in China found that children and adults were just as likely to be infected.
Initial estimates of the basic reproduction number (R0) for COVID-19 in January were between 1.4 and 2.5, but a subsequent analysis concluded that it might be about 5.7 (with a 95 percent confidence interval of 3.8 to 8.9). R0 can vary across populations and is not confused with the effective reproduction number (commonly just called R), which considers effects such as social distancing and herd immunity. By mid-May 2020, the effective R was close to or below 1.0 in many countries, meaning the spread of the disease in these areas at that time was stable or decreasing.
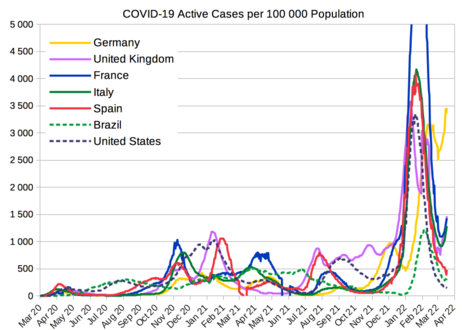
Deaths
Deceased in a 16 m (53 ft) “mobile morgue” outside a hospital in Hackensack, New Jersey, USA
Official deaths from COVID-19 generally refer to people who died after testing positive according to protocols. These counts may ignore the deaths of people who die without having been tested. Conversely, deaths of people who had underlying conditions may lead to over-counting. Comparisons of statistics for deaths for all causes versus the seasonal average indicate excess mortality in many countries. This may include deaths due to strained healthcare systems and bans on elective surgery. The first confirmed death was in Wuhan on 9 January 2020. According to The Washington Post, on 7 July 2021, patient zero (S01) was an accountant in Wuhan who began feeling ill on 8 December 2019. Nevertheless, the first reported death outside of China occurred on 1 February 2020 in the Philippines, and the first reported death outside Asia was in the United States on 6 February 2020.
More than 95 percent of the people who contract COVID-19 recover. Otherwise, the time between symptoms onset and death usually ranges from 6 to 41 days, typically about 14 days. As of 8 July 2021, more than 4 million deaths have been attributed to COVID-19. People at the greatest risk of mortality from COVID-19 tend to be those with underlying conditions, such as those with a weakened immune system, serious heart or lung problems, severe obesity, or the elderly (including individuals age 65 years or older). Multiple measures are used to quantify mortality. These numbers vary by region and over time, influenced by testing volume, healthcare system quality, treatment options, government response, time since the initial outbreak, and population characteristics, such as age, sex, and overall health. Countries like Belgium include deaths from suspected cases of COVID-19, regardless of whether the person was tested, resulting in higher numbers compared to countries that include only test-confirmed cases. The death-to-case ratio reflects the number of deaths attributed to COVID-19 divided by the number of diagnosed cases within a given time interval. Based on Johns Hopkins University statistics, the global death-to-case ratio is 2.2 percent (4,001,791 deaths for 185,078,882 cases) as of 8 July 2021. The number varies by region.
-
COVID-19 deaths per 100 000 population from selected countries. The official death counts have been criticized for underreporting the actual death toll because comparisons of death rates before and during the pandemic show an increase in deaths that is not explained by COVID-19 deaths alone. Using such data, estimates of the true number of deaths from COVID-19 worldwide have included a range from 7 to 13 million by The Economist and over 9 million by the Institute for Health Metrics and Evaluation.
Reporting
On 24 March 2020, the Centers for Disease Control and Prevention (CDC) of the United States indicated the WHO had provided two codes for COVID-19: U07.1 when confirmed by laboratory testing and U07.2 for clinically or epidemiological diagnosis where laboratory confirmation is inconclusive or not available. The CDC noted that “Because laboratory test results are not typically reported on death certificates in the U.S., [the National Center for Health Statistics (NCHS)] is not planning to implement U07.2 for mortality statistics” and that U07.1 would be used “If the death certificate reports terms such as ‘probable COVID-19’ or ‘likely COVID-19’.” The CDC also noted, “It Is not likely that NCHS will follow up on these cases,” and while the “underlying cause depends upon what and where conditions are reported on the death certificate, … the rules for coding and selection of the … cause of death are expected to result in COVID–19 being the underlying cause more often than not.
On 16 April 2020, the WHO, in its formal publication of the two codes, U07.1 and U07.2, “recognized that in many countries detail as to the laboratory confirmation… will not be reported [and] recommended, for mortality purposes only, to code COVID-19 provisionally to code U07.1 unless it is stated as ‘probable’ or ‘suspected.’ It was also noted that the WHO “does not distinguish” between infection by SARS-CoV-2 and COVID-19.
Infection fatality ratio (IFR)
| Coronaviruses |
|---|
 |
A crucial metric in assessing the severity of a disease is the infection fatality ratio (IFR), which is the cumulative number of deaths attributed to the disease divided by the cumulative number of infected individuals (including asymptomatic and undiagnosed infections) as measured or estimated as of a specific date. Epidemiologists frequently refer to this metric as the ‘infection fatality rate’ to clarify that it is expressed in percentage points (not as a decimal). Other published studies refer to this metric as the ‘infection fatality risk.’
In November 2020, a review article in Nature reported estimates of population-weighted IFRs for several countries, excluding deaths in elderly care facilities, and found a median range of 0.24% to 1.49%.
In December 2020, a systematic review and meta-analysis published in the European Journal of Epidemiology estimated that population-weighted IFR was 0.5% to 1% in some countries (France, Netherlands, New Zealand, and Portugal), 1% to 2% in several other countries (Australia, England, Lithuania, and Spain), and about 2.5% in Italy; these estimates included fatalities in elderly care facilities. This study also found that most of the differences in IFR across locations reflected corresponding differences in the age composition of the population and the age-specific pattern of infection rates due to very low IFRs for children and younger adults (e.g., 0.002% at age 10 and 0.01% at age 25) and progressively higher IFRs for older adults (0.4% at age 55, 1.4% at age 65, 4.6% at age 75, and 15% at age 85). These results were also highlighted in a December 2020 report issued by the World Health Organization.
| Age group | IF |
|---|---|
| 0–34 | 0.004% |
| 35–44 | 0.068% |
| 45–54 | 0.23% |
| 55–64 | 0.75% |
| 65–74 | 2.5% |
| 75–84 | 8.5% |
| 85 + | 28.3% |
An analysis of those IFR rates indicates that COVID-19 is hazardous not only for the elderly but also for middle-aged adults. A fatal COVID-19 infection is two orders of magnitude more likely than the annualized risk of a fatal automobile accident and far more dangerous than seasonal influenza.
Case fatality ratio (CFR)
Another metric in assessing the death rate is the case fatality ratio (CFR), which is deaths attributed to a disease divided by individuals diagnosed to date. This metric can be misleading because of the delay between symptom onset and death and because testing focuses on individuals with symptoms (particularly on those manifesting more severe symptoms). On 4 August 2020, WHO indicated “at this early stage of the pandemic, most estimates of fatality ratios have been based on cases detected through surveillance and calculated using crude methods, giving rise to widely variable estimates of CFR by country – from less than 0.1% to over 25%.
Disease
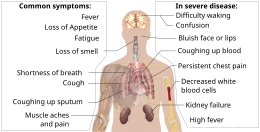
Signs and symptoms
Symptoms of COVID-19
Symptoms of COVID-19 are variable, ranging from mild symptoms to severe illness. Common symptoms include headache, loss of smell and taste, nasal congestion and runny nose, cough, muscle pain, sore throat, fever, diarrhea, and breathing difficulties. People with the same infection may have different symptoms, and their symptoms may change over time. Three common clusters of symptoms have been identified: one respiratory symptom cluster with cough, sputum, shortness of breath, and fever; a musculoskeletal symptom cluster with muscle and joint pain, headache, and fatigue; a cluster of digestive symptoms with abdominal pain, vomiting, and diarrhea. In people without the prior ear, nose, and throat disorders, loss of taste combined with the loss of smell is associated with COVID-19. Of people who show symptoms, 81% develop only mild to moderate symptoms (up to mild pneumonia). In comparison, 14% develop severe symptoms (dyspnea, hypoxia, or more than 50% lung involvement on imaging), and 5% of patients suffer critical symptoms (respiratory failure, shock, or multiorgan dysfunction). At least a third of the infected people do not develop noticeable symptoms at any point in asymptomatic carriers tend not to get tested and can spread the disease. Other infected people will develop symptoms later, called “pre-symptomatic,” or have very mild symptoms and spread the virus. As is common with infections, there is a delay between the moment a person first becomes infected and the appearance of the first symptoms. The median delay for COVID-19 is four to five days. Most symptomatic people experience symptoms within two to seven days after exposure, and almost all will experience at least one symptom within 12 days.
Most people recover from the acute phase of the disease. However, some people continue to experience a range of effects for months after recovery—named long COVID—and damage to organs has been observed. Multi-year studies are underway to investigate the long-term effects of the disease further.
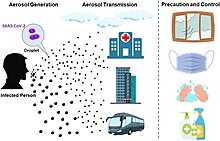
Transmission
The disease is mainly transmitted via the respiratory route when people inhale droplets and particles that infected people release as they breathe, talk, cough, sneeze, or sing. Infected people are more likely to transmit COVID-19 when they are physically close. However, the infection can occur over longer distances, particularly indoors.
Infectivity begins as early as three days before symptoms appear, and people are most infectious just before and during the onset of symptoms. It declines after the first week, but infected people remain contagious for up to 20 days. People can spread the disease even if they are asymptomatic.
Infectious particles range in size from aerosols that remain suspended in the air for long periods of time to larger droplets that remain airborne or fall to the ground. Various groups utilize terms such as “airborne” and “droplet” in technical and general ways, leading to confusion around terminology. Additionally, COVID-19 research has redefined the traditional understanding of how respiratory viruses transmit. The largest droplets of respiratory fluid do not travel far and can be inhaled or land on mucous membranes on the eyes, nose, or mouth to infect. Aerosols are highest in concentration when people are nearby, which leads to the easier viral transmission when people are physically close, but airborne transmission can occur at longer distances, mainly in locations that are poorly ventilated; in those conditions, small particles can remain suspended in the air for minutes to hours.
The number of people generally infected by one infected person varies, as only 10 to 20% of people are responsible for the diseases spread. It often spreads in clusters, where infections can be traced back to an index case or geographical location. Often in these instances, superspreading events occur, where one person infects many people.
Cause
Illustration of SARS-CoV-2 virion
SARS‑CoV‑2 belongs to the broad family of viruses known as coronaviruses. It is a positive-sense single-stranded RNA (+ssRNA) virus with a single linear RNA segment. Coronaviruses infect humans, other mammals, and avian species, including livestock and companion animals. Human coronaviruses are capable of causing illnesses ranging from the common cold to more severe diseases such as the Middle East respiratory syndrome (MERS, fatality rate ~34%). SARS-CoV-2 is the seventh known coronavirus to infect people, after 229E, NL63, OC43, HKU1, MERS-CoV, and the original SARS-CoV.
Viral genetic sequence data can provide critical information about whether viruses separated by time and space are likely to be epidemiologically linked. With a sufficient number of sequenced genomes, it is possible to reconstruct a phylogenetic tree of the mutation history of a family of viruses. By 12 January 2020, five genomes of SARS‑CoV‑2 were isolated from Wuhan and reported by the Chinese Center for Disease Control and Prevention (CCDC) and other institutions; the number of genomes increased to 42 30 January 2020. A phylogenetic analysis of those samples showed they were “highly related with at most seven mutations relative to a common ancestor,” implying that the first human infection occurred in November or December 2019. Examination of the topology of the phylogenetic tree at the start of the pandemic also found high similarities between human isolates. As of 7 May 2020, 4,690 SARS‑CoV‑2 genomes sampled on six continents were publicly available.
Diagnosis
Demonstration of a nasopharyngeal swab for COVID-19 testing
The standard methods of testing for SARS-CoV-2 are nucleic acid tests, which detect the presence of viral RNA fragments. As these tests detect RNA but not an infectious virus, its “ability to determine the duration of infectivity of patients is limited. The test is typically done on respiratory samples obtained by a nasopharyngeal swab; however, a nasal swab or sputum sample may also be used. Results are generally available within hours—the WHO has published several testing protocols for the disease.
Prevention
Preventive measures to reduce the chances of infection include getting vaccinated, staying at home, wearing a mask in public, avoiding crowded places, keeping distance from others, ventilating indoor spaces, managing potential exposure durations, washing hands with soap and water often and for at least twenty seconds, practicing good respiratory hygiene, and avoiding touching the eyes, nose, or mouth with unwashed hands.
The CDC advises those diagnosed with COVID-19 or who believe they may be infected to stay home except to get medical care, call ahead before visiting a healthcare provider, wear a face mask before entering the healthcare provider’s office, and when in any room or vehicle with another person, cover coughs and sneezes with a tissue, regularly wash hands with soap and water and avoid sharing personal household items.
Vaccines
A doctor at Walter Reed National Military Medical Center receiving a COVID-19 vaccination
On 21 December 2020, the European Union approved the Pfizer BioNTech vaccine. Vaccinations began to be administered on 27 December 2020. The Moderna vaccine was authorized on 6 January 2021, and the AstraZeneca vaccine was authorized on 29 January 2021.
On 4 February 2020, US Secretary of Health and Human Services Alex Azar published a notice of declaration under the Public Readiness and Emergency Preparedness Act for medical countermeasures against COVID-19, covering “any vaccine, used to treat, diagnose, cure, prevent, or mitigate COVID-19, or the transmission of SARS-CoV-2 or a virus mutating therefrom”, and stating that the declaration precludes “liability claims alleging negligence by a manufacturer in creating a vaccine, or negligence by a health care provider in prescribing the wrong dose, absent willful misconduct.” The declaration is effective in the United States through 1 October 2024. On 8 December, it was reported that the AstraZeneca vaccine is about 70% effective, according to a study.
By mid-June 2021, 85 percent of vaccinations have been administered in high- and upper-middle-income countries. Only 0.3 percent of doses have been administered in low-income countries.
Treatment
There is no specific, effective treatment or cure for coronavirus disease 2019 (COVID-19), the disease caused by the SARS-CoV-2 virus. Thus, the cornerstone of management of COVID-19 is supportive care, which includes treatment to relieve symptoms, fluid therapy, oxygen support, prone positioning as needed, and medications or devices to support other affected vital organs.
A critically ill patient receiving invasive ventilation in the intensive care unit of the Heart Institute, University of São Paulo. Due to a shortage of mechanical ventilators, a bridge ventilator is being used to actuate a bag valve mask automatically.
Most cases of COVID-19 are mild. In these, supportive care includes paracetamol or NSAIDs to relieve symptoms (fever, body aches, cough), proper intake of fluids, rest, and nasal breathing. Good personal hygiene and a healthy diet are also recommended. The U.S. Centers for Disease Control and Prevention (CDC) recommend that those who suspect they carry the virus isolate themselves at home and wear a face mask. People with more severe cases may need treatment in hospitals. In those with low oxygen levels, glucocorticoid dexamethasone is strongly recommended, as it can reduce the risk of death. Noninvasive ventilation and, ultimately, admission to an intensive care unit for mechanical ventilation may be required to support breathing. Extracorporeal membrane oxygenation (ECMO) has been used to address the issue of respiratory failure, but its benefits are still under consideration.
Several experimental treatments are being actively studied in clinical trials. Others were thought to be promising early in the pandemic, such as hydroxychloroquine and lopinavir/ritonavir, but later research found them ineffective or even harmful. Despite ongoing research, there is still not enough high-quality evidence to recommend so-called early treatment. Nevertheless, in the United States, two monoclonal antibody-based therapies are available for early use in cases thought to be at high risk of progression to severe disease. The antiviral redeliver is available in the U.S., Canada, Australia, and several other countries, with varying restrictions; however, it is not recommended for people needing mechanical ventilation and is discouraged altogether by the World Health Organization (WHO), due to limited evidence of its efficacy.
Variants
Several variants of SARS-CoV-2 have emerged that are spreading globally. The most currently prevalent, all of which share the more infectious D614G mutation, are:
- B.1.1.7, also known as the Alpha variant, first detected in the UK, which has spread to over 120 countries
- P.1, also known as the Gamma variant, first detected in Brazil, which has spread to more than 50 countries
- B.1.351, also known as the Beta variant, first detected in South Africa, which has spread to over 80 countries
- B.1.617.2, also known as the Delta variant, first detected in India, which has spread to over 70 countries
Prognosis
The severity of COVID-19 varies. The disease may take a mild course with few or no symptoms, resembling other common upper respiratory diseases like the common cold. In 3–4% of cases (7.4% for those over age 65), symptoms are severe enough to cause hospitalization. Mild cases typically recover within two weeks, while those with severe or critical diseases may take three to six weeks to recover. Among those who have died, the time from symptom onset to death has ranged from two to eight weeks. The Italian Istituto Superiore di Sanità reported that the median time between the onset of symptoms and death was twelve days, with seven being hospitalized. However, people transferred to an ICU had a median time of ten days between hospitalization and death. Prolonged prothrombin time and elevated C-reactive protein levels on admission to the hospital are associated with a severe course of COVID-19 and with a transfer to ICU.
Mitigation
Speed and scale are key to mitigation due to the fat-tailed nature of pandemic risk and the exponential growth of COVID-19 infections. For mitigation to be effective, (a) chains of transmission must be broken as quickly as possible through screening and containment, (b) health care must be available to provide for the needs of those infected, and (c) contingencies must be in place to allow for the effective rollout of (a) and (b).
Screening, containment, and mitigation
Goals of mitigation include delaying and reducing peak burden on healthcare (flattening the curve) and lessening overall cases and health impact. Moreover, progressively greater increases in healthcare capacity (raising the line) such as increasing bed count, personnel, and equipment help meet increased demand.
The CDC and WHO advises that masks (such as worn here by Taiwanese president Tsai Ing-wen) reduce the spread of SARS-CoV-2.
Strategies in the control of an outbreak are screening, containment (or suppression), and mitigation. Screening is done with a device such as a thermometer to detect the elevated body temperature associated with fevers caused by the infection. Containment is undertaken in the early stages of the outbreak and aims to trace and isolate those infected and introduce other measures to stop the disease from spreading. When it is no longer possible to contain the disease, efforts then move to the mitigation stage: measures are taken to slow the spread and mitigate its effects on the healthcare system and society. A combination of both containment and mitigation measures may be undertaken at the same time. Suppression requires more extreme measures to reverse the pandemic by reducing the basic reproduction number to less than 1.
Managing an infectious disease outbreak is trying to delay and decrease the epidemic peak, known as flattening the epidemic curve. This decreases the risk of health services being overwhelmed and provides more time for vaccines and treatments to be developed. Non-pharmaceutical interventions that may manage the outbreak include personal preventive measures such as hand hygiene, wearing face masks, and self-quarantine; community measures aimed at physical distancing such as closing schools and canceling mass gathering events; community engagement to encourage acceptance and participation in such interventions; as well as environmental measures such surface cleaning. Some measures, particularly those focusing on cleaning surfaces rather than preventing airborne transmission, have been criticized as hygiene theatre.
More drastic actions aimed at containing the outbreak were taken in China once the outbreak’s severity became apparent, such as quarantining entire cities and imposing strict travel bans. Other countries also adopted a variety of measures aimed at limiting the spread of the virus. South Korea introduced mass screening and localized quarantines and issued alerts on the movements of infected individuals. Singapore provided financial support for those infected who quarantined themselves and imposed large fines for those who failed to do so. Taiwan increased face mask production and penalized the hoarding of medical supplies.
Simulations for Great Britain and the United States show that mitigation (slowing but not stopping epidemic spread) and suppression (reversing epidemic growth) have major challenges. Optimal mitigation policies might reduce peak healthcare demand by two-thirds and deaths by half but still result in hundreds of thousands of deaths and overwhelmed health systems. Suppression can be preferred but needs to be maintained for as long as the virus is circulating in the human population (or until a vaccine becomes available), as transmission otherwise quickly rebounds when measures are relaxed. Long-term intervention to suppress the pandemic has considerable social and economic costs.
Contact tracing

Mandatory traveler information collection for use in COVID-19 contact tracing at New York City’s LaGuardia Airport in August 2020
Contact tracing is an important method for health authorities to determine the source of infection and to prevent further transmission. The use of location data from mobile phones by governments for this purpose has prompted privacy concerns, with Amnesty International and more than a hundred other organizations issuing a statement calling for limits on this kind of surveillance.
Several mobile apps have been implemented or proposed for voluntary use. As of 7 April 2020, more than a dozen expert groups were working on privacy-friendly solutions such as using Bluetooth to log users’ proximity to other cellphones. (Users are alerted if they have been near someone who subsequently tests positive.)
On 10 April 2020, Google and Apple jointly announced an initiative for privacy-preserving contact tracing based on Bluetooth technology and cryptography. The system intends to allow governments to create official privacy-preserving coronavirus tracking apps, with the eventual goal of integrating this functionality directly into the iOS and Android mobile platforms. In Europe and the U.S., Palantir Technologies is also providing COVID-19 tracking services.
Health care
An army-constructed field hospital outside Östra sjukhuset (Eastern hospital) in Gothenburg, Sweden, contains temporary intensive care units for COVID-19 patients.
Increasing capacity and adapting healthcare for the needs of COVID-19 patients is described by the WHO as a fundamental outbreak response measure. The ECDC and the European regional office of the WHO have issued guidelines for hospitals and primary healthcare services for shifting of resources at multiple levels, including focusing laboratory services towards COVID-19 testing, canceling elective procedures whenever possible, separating and isolating COVID-19 positive patients, and increasing intensive care capabilities by training personnel and increasing the number of available ventilators and beds. In addition, in an attempt to maintain physical distancing and protect both patients and clinicians, non-emergency healthcare services are being provided virtually in some areas.
Due to capacity limitations in the standard supply chains, some manufacturers are 3D printing healthcare materials such as nasal swabs and ventilator parts. In one example, when an Italian hospital urgently required a ventilator valve, and the supplier could not deliver in the timescale required, a local startup received legal threats due to alleged patent infringement after reverse-engineering and printing the required hundred valves overnight. On 23 April 2020, NASA reported building, in 37 days, a ventilator that is currently undergoing further testing. NASA is seeking fast-track approval. Individuals and groups of makers worldwide also assisted in creating and sharing open-source designs and manufacturing devices using locally sourced materials, sewing, and 3D printing. Millions of face shields, protective gowns, and masks were made. Other medical supplies were made, such as shoe covers, surgical caps, powered air-purifying respirators, and hand sanitizer. Novel devices were created, such as ear savers, non-invasive ventilation helmets, and ventilator splitters.
History
2019
The Huanan Seafood Wholesale Market in March 2020, after it was closed down.
Based on the retrospective analysis, starting from December 2019, the number of COVID-19 cases in Hubei gradually increased, reaching 60 by 20 December and at least 266 by 31 December.
On 24 December 2019, Wuhan Central Hospital sent a bronchoalveolar lavage fluid (BAL) sample from an unresolved clinical case to sequencing company Vision Medicals. On 27 and 28 December, Vision Medicals informed the Wuhan Central Hospital and the Chinese CDC of the test results, showing a new coronavirus. A pneumonia cluster of unknown cause was observed on 26 December and treated by the doctor Zhang Jixian in Hubei Provincial Hospital, who informed the Wuhan Jianghan CDC on 27 December.
On 30 December 2019, a test report addressed to Wuhan Central Hospital, from company CapitalBio Medlab, stated an erroneous positive result for SARS, causing a group of doctors at Wuhan Central Hospital to alert their colleagues and relevant hospital authorities of the result. Eight of those doctors, including Li Wenliang (who was also punished on 3 January), were later admonished by the police for spreading false rumors; and another doctor, Ai Fen, was reprimanded by her superiors for raising the alarm. That evening, the Wuhan Municipal Health Commission issued a notice to various medical institutions about “the treatment of pneumonia of unknown cause.” The next day, the Wuhan Municipal Health Commission made the first public announcement of a pneumonia outbreak of unknown cause, confirming 27 cases enough to trigger an investigation.
The following day, on 31 December, the WHO office in China was informed of cases of pneumonia of unknown cause in Wuhan. An investigation was launched at the start of January 2020.
According to official Chinese sources, the early cases were mostly linked to the Huanan Seafood Wholesale Market, which also sold live animals. However, in May 2020, George Gao, the Chinese Center for Disease Control and Prevention director, said animal samples collected from the seafood market had tested negative for the virus, indicating the market was not the source of the initial outbreak. In March 2021, the WHO published its report on the potential zoonotic source of the virus. The WHO concluded that human spillover via an intermediate animal host was the most likely explanation, with direct spillover from bats next most likely and introduction through the food supply chain as another possible explanation.
2020
Chinese medics in the city of Huanggang, Hubei on 20 March 2020
From 31 December 2019 to 3 January 2020, a total of 44 cases of “pneumonia of unknown causes” were reported to WHO by the Chinese authorities.
On 11 January, WHO received further information from the Chinese National Health Commission that the outbreak is associated with exposures in one seafood market in Wuhan. The Chinese authorities had identified a new type of coronavirus, which was isolated on 7 January.
During the early stages of the outbreak, the number of cases doubled by approximately seven and a half days. In early and mid-January, the virus spread to other Chinese provinces, helped by the Chinese New Year migration and Wuhan being a transport hub and major rail interchange. On 10 January, the SARS-CoV-2 genetic sequence data was shared through GISAID. On 20 January, China reported nearly 140 new cases in one day, including two people in Beijing and one in Shenzhen. A retrospective official study published in March found that 6,174 people had already developed symptoms by 20 January (most of them would be diagnosed later), and more may have been infected. A report in The Lancet on 24 January indicated human transmission strongly recommended personal protective equipment for health workers and said testing for the virus was essential due to its “pandemic potential.” On 31 January, The Lancet would publish the first modeling study explicitly warning of inevitable “independent, self-sustaining outbreaks in major cities globally” and calling for “large-scale public health interventions.
On 30 January, with 7,818 confirmed cases across 19 countries, the WHO declared the COVID-19 outbreak a Public Health Emergency of International Concern (PHEIC), and then a pandemic on 11 March 2020 as Italy, Iran, South Korea, and Japan reported increasing numbers of cases.
On 31 January, Italy had its first confirmed cases, two tourists from China. On 19 March, Italy overtook China as the country with the most reported deaths. By 26 March, the United States had overtaken China and Italy with the highest number of confirmed cases globally. Research on SARS-CoV-2 genomes indicates that most COVID-19 cases in New York came from European travelers rather than directly from China or any other Asian country. Retesting of prior samples found a person in France who had the virus on 27 December 2019\ and a person in the United States who died from the disease on 6 February 2020.
A patient in Ukraine in May 2020 wears a scuba mask in the absence of artificial ventilation.
On 11 June, after 55 days without a locally transmitted case being officially reported, the city of Beijing reported a single COVID-19 case, followed by two more cases on 12 June. As of 15 June 2020, 79 cases were officially confirmed. Most of these patients went to Xinfadi Wholesale Market.
On 29 June, WHO warned that the spread of the virus was still accelerating as countries reopened their economies, despite many countries have made progress in slowing down the spread.
On 15 July, one COVID-19 case was officially reported in Dalian in more than three months. The patient did not travel outside the city in the 14 days before developing symptoms, nor did he contact people from “areas of attention.
In October, the WHO stated, at a special meeting of WHO leaders, that one in ten people around the world may have been infected with COVID-19. At the time, that translated to 780 million people being infected, while only 35 million infections had been confirmed.
In early November, Denmark reported an outbreak of a unique mutated variant being transmitted to humans from minks in its North Jutland Region. All twelve human cases of the mutated variant were identified in September 2020. The WHO released a report saying the variant “had a combination of mutations or changes that have not been previously observed. In response, Prime Minister Mette Frederiksen ordered the country – the world’s largest producer of mink fur – to cull its mink population by as many as 17 million. On 9 November, Pfizer released their trial results for a candidate vaccine, showing that it is 90% effective against the virus. Later that day, Novavax entered an FDA Fast Track application for their vaccine. Virologist and U.S. National Institute of Allergy and Infectious Diseases director Anthony Fauci indicated that the Pfizer vaccine targets the spike protein used to infect cells by the virus. Some issues left to be answered how long the vaccine offers protection and if it offers the same level of protection to all ages. Initial doses will likely go to healthcare workers on the front lines.
On 9 November 2020, the United States surpassed 10 million confirmed cases of COVID-19, making it the country with the most cases worldwide by a large margin.
It was reported on 27 November that a publication released by the Centers for Disease Control and Prevention indicated that the current numbers of viral infections are via confirmed laboratory tests only. However, the true number could be about eight times the reported number; the report further indicated that the true number of virus-infected cases could be around 100 million in the U.S.
On 14 December, Public Health England reported a new variant had been discovered in the South East of England, predominantly in Kent. The variant, named Variant of Concern 202012/01, showed changes to the spike protein, making the virus more infectious. As of 13 December, there were 1,108 cases identified. Many countries halted all flights from the UK; France-bound Eurotunnel service was suspended. Ferries carrying passengers and accompanied freight were canceled as the French border closed to people on 20 December.
2021
On 2 January, VOC-202012/01, a variant of SARS-CoV-2 first discovered in the UK, had been identified in 33 countries around the world, including Pakistan, South Korea, Switzerland, Taiwan, Norway, Italy, Japan, Lebanon, India, Canada, Denmark, France, Germany, Iceland, and China.
On 6 January, the P.1 variant was first identified in Japanese travelers who had just returned from Brazil.
On 12 January, it was reported that a team of scientists from the World Health Organization would arrive in Wuhan on the 14th of the month; this is to ascertain the origin of SARS-CoV-2 and determine what the intermediate hosts between the original reservoir and humans were. On the following day, two of the WHO members were barred from entering China because, according to the country, antibodies for the virus were detected in both. On 29 January, it was reported that the Novavax vaccine was only 49% effective against the 501.V2 variant in a clinical trial in South Africa. The China COVID-19 vaccine CoronaVac indicated 50.4% effectivity in a Brazilian clinical trial.
On 12 March, several countries, including Thailand, Denmark, Bulgaria, Norway, and Iceland, had stopped using the Oxford-AstraZeneca COVID-19 vaccine due to what was being called severe blood clotting problems a cerebral venous sinus thrombosis (CVST). Additionally, Austria halted the use of one batch of the aforementioned vaccine as well. On 20 March, the WHO and European Medicines Agency found no link between thrombus (a blood clot of clinical importance), leading several European countries to resume administering the AstraZeneca vaccine.
On 29 March, it was reported that the U.S. government was planning to introduce COVID-19 vaccination ‘passports’ to allow those who have been vaccinated the ability to board airplanes, cruise ships as well as other activities. As of 8 July 2021, more than 185 million cases have been reported worldwide due to COVID-19; more than 4 million have died.
National responses
Then-US President Donald Trump signs the Coronavirus Preparedness and Response Supplemental Appropriations Act into law with Alex Azar on 6 March 2020.
Due to the pandemic in Europe, many countries in the Schengen Area have restricted free movement and set up border controls. National reactions have included containment measures such as quarantines and curfews (known as stay-at-home orders, shelter-in-place orders, or lockdowns). The WHO’s recommendation on curfews and lockdowns should be short-term measures to reorganize, regroup, rebalance resources, and protect health workers who are exhausted. To achieve a balance between restrictions and normal life, the long-term responses to the pandemic should consist of strict personal hygiene, effective contact tracing, and isolating when ill. By 26 March 2020, 1.7 billion people worldwide were under some form of lockdown, which increased to 3.9 billion people by the first week of April—more than half the world’s population.
By late April 2020, around 300 million people were under lockdown in nations of Europe, including but not limited to Italy, Spain, France, and the United Kingdom, while around 200 million people were under lockdown in Latin America. Nearly 300 million people, or about 90 percent of the population, were under some form of lockdown in the United States, around 100 million people in the Philippines, about 59 million people in South Africa, and 1.3 billion people have been under lockdown in India.
Asia
As of 30 April 2020, cases have been reported in all Asian countries except Turkmenistan and North Korea, although these countries likely also have cases. Despite being the first area of the world hit by the outbreak, the early wide-scale response of some Asian states, particularly Bhutan, Singapore, Taiwan, and Vietnam, has allowed them to fare comparatively well. China is criticized for initially minimizing the severity of the outbreak, but the delayed wide-scale response has largely contained the disease since March 2020.
In Japan, the pandemic has been believed to have caused direct side effects regarding mental health. According to the country’s National Police Agency report, suicides had increased to 2,153 in October. Experts also state that the pandemic has worsened mental health issues due to lockdowns and isolation from family members, among other issues.
China
A temporary hospital constructed in Wuhan in February 2020
As of 14 July 2020, there are 83,545 cases confirmed in China—excluding 114 asymptomatic cases, 62 of which were imported, under medical observation; asymptomatic cases have not been reported before 31 March 2020—with 4,634 deaths 78,509 recoveries, meaning there are only 402 cases. Hubei has the most cases, followed by Xinjiang. By March 2020, COVID-19 infections have largely been put under control in China, with minor outbreaks since. It was reported on 25 November that some 1 million people in the country of China had been vaccinated according to China’s state council; the vaccines against COVID-19 come from Sinopharm, which makes two and one produced by Sinovac.
India
Indian officials conducting temperature checks at the Ratha Yatra Hindu festival on 23 June 2020
The first case of COVID-19 in India was reported on 30 January 2020. India ordered a nationwide lockdown for the entire population starting 24 March 2020, with a phased unlock beginning 1 June 2020. Six cities account for around half of all reported cases in Mumbai, Delhi, Ahmedabad, Chennai, Pune, and Kolkata. On 10 June 2020, India’s recoveries exceeded active cases for the first time.
On 30 August 2020, India surpassed the US record for the most cases in a single day, with more than 78,000 cases, and set a new record on 16 September 2020, with almost 98,000 cases reported that day. As of 30 August 2020, India’s case fatality rate is relatively low at 2.3%, against the global 4.7%.
As of September 2020, India had the largest number of confirmed cases in Asia. The second-highest number of confirmed cases in the world, behind the United States, with the number of totals confirmed cases breaching the 100,000 marks on 19 May 2020, 1,000,000 on 16 July 2020, and 5,000,000 confirmed cases on 16 September 2020.
On 19 December 2020, India crossed the total number of 10,000,000 confirmed cases but at a slow pace.
The Indian Ministry of Science initiated a mathematical simulation of the pandemic, the so-called “Indian Supermodel,” which correctly predicted the decrease of active cases starting in September 2020.
A second wave hit India in April 2021, placing healthcare services under severe strain. By late April, the government reported over 300,000 new infections and 2,000 deaths per day, with concerns of undercounting.
https://www.who.int/emergencies/diseases/novel-coronavirus-2019





































2 thoughts on "novel coronavirus-2019 Covid-19"